PERIVASCULAR ADIPOSE TISSUE: A NOVEL COMPONENT OF GLOBAL
CARDIOMETABOLIC RISK
1Mariyana G. Hristova, MD, PhD; 3Plamen Panayotov, MD; 4Luigi Aloe, PhD
1Division of Cell Biology, Medical University, Varna, Bulgaria
2Department of General and Clinical Pathology, Medical University, Varna, Bulgaria
3Cardiovascular Surgery Clinic, University St Marina Hospital, Varna, Bulgaria
4Institute of Neurobiology and Molecular Medicine, National Research Council, Rome, Italy
chaldakov@yahoo.com

Key Points
- Perivascular adipose tissue (tunica adipose) is considered a novel component of global cardiometabolic risk.
- Hence, not only intima-media and epicardial/pericardial adipose tissue thickness, but also tunica adipose thickness, should be evaluated in identifying high-risk populations susceptible to cardiovascular disease and monitor vascular wall changes during follow-up studies and therapeutic trials.
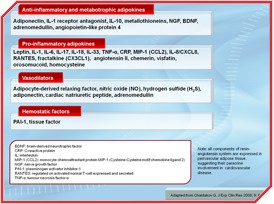
Recently, obesity and related cardiovascular disease (CVD) are among the major physical, social and economic burdens, globally. The World Health Organization has predicted a "globesity epidemic" with more than one billion adults being overweight (body mass index [BMI] =25 kg/m2) and at least 400 million of these being clinically obese (BMI =30 kg/m2). Arguably, we have learned more about the molecular control of food intake and energy homeostasis, particularly, the role played by adipose tissue in the pathogenesis of various diseases, including CVD. Atherogenic stimuli such as inflammation, endothelial dysfunction, hemostatsis, and smooth muscle cell growth are influenced by adipose tissue-secreted signalling proteins, collectively termed adipokines (Table). Cumulatively, such an adipocentric approach has integrated the traditional cardiovascular risk factors (age, sex, smoking, hypertension, dyslipidemia, homocysteinemia) and intra-abdominal (visceral) obesity and related features of the metabolic syndrome, hence, global cardiometabolic risk [1-3].
The Road Less Traveled1
The prevailing response-to-injury hypothesis of Russell Ross states that atherosclerosis is an inflammatory disease, leading to intimal lesions and luminal loss [4]; that is, the intimal road to atherogenesis. Accordingly, intima-media thickness became an accepted measure of structural vascular remodelling and a strong predictor of CVD. However, it is unlikely that such a road may solely travel the whole multiplex network like that of atherogenesis. An interactive approach targeting all structural components of the vascular wall was required [5-6].
Large- and medium-sized blood vessels, where usually atherosclerosis develops, are surrounded by perivascular adipose tissue (PVAT). Hence, adipokines, via a paracrine way, may contribute to different pro- and anti-atherogenic events [7-11]. Pharmacological studies aimed at modifying the production and/or receptor sensitivity of PVAT-derived adipokines are required.
 [Click to enlarge]
[Click to enlarge]
Given the key role of inflammation in the development of atherosclerotic lesions, what role might PVAT play in the process of atherogenesis? For instance, it is known that the proximal segments of coronary arteries are surrounded by subepicardial adipose tissue, and these segments are atherosclerosis-prone as compared to the distal, intramyocardial, adiposa-free segments, which are atherosclerosis-resistant [5-6]. However, the removal of PVAT enhances neointima formation after injury, which is attenuated by transplantation of subcutaneous adipose tissue [9]. Likewise, high-fat feeding induces inflammation and decreases adiponectin expression in PVAT resulting in neointima formation, which is inhibited by local application of adiponectin [9].
In effect, PVAT, recently designated tunica adiposa [11], may be a novel component of global cardiometabolic risk. Therefore, not only intima-media and epicardial/pericardial adipose tissue thickness [11-14], but also, adiposa thickness should be evaluated in, for example, identifying high-risk population susceptible to CVD and monitor vascular wall changes during follow-up studies and therapeutic trials [15-16].
Conclusion
Traditional concept of atherogenesis focuses on the intimal road, where "inside-out" inflammatory processes and endothelial dysfunction trigger atherosclerotic plaque formation. Here we took the adipose road, which is less traveled1 , focusing on the possible paracrine role of PVAT in an "outside-in" signalling pathway in CVD [5-7, 9-11]; its role in insulin resistance should also be considered [8].
Until recently, physicians have looked upon obesity as accumulation of external adipose tissue. This was routinely evaluated by various anthropometic measurements including BMI and waist, hip and, recently, neck circumference. However, recent noninvasive techniques, such as echography, computed tomography, magnetic resonance imaging and positron emission tomography, reveal a new picture of adipose tissue distribution [17]. Hence, in global cardiometabolic risk, we should appreciate not only anthropometric values of external adipose tissue, but - more importantly - the "weight" of internal adipose tissue, particularly, PVAT as well as epicardial and pericardial adipose tissue [11-14]. Metabolic-cognitive association [18-19] might also be listed in global cardiometabolic risk.
- Frost R. (1874-1963) from his poem The road not taken:
Two roads diverged in a wood, and I
-I took the one less traveled by,
And that has made all the difference.
References
- Vanuzzo D, Pilotto L, Mirolo R, et al. [Cardiovascular risk and cardiometabolic risk: an epidemiological evaluation]. G Ital Cardiol (Rome) 2008; 9: 6S-17S.
- Shimabukuro M. Cardiac adiposity and global cardiometabolic risk: new concept and clinical implication. Circ J 2009; 73: 27-34.
- Després JP, Arsenault BJ, Côté M, et al. Abdominal obesity: the cholesterol of the 21st century? Can J Cardiol 2008; 24 Suppl D: 7D-12D.
- Ross R. Atherosclerosis--an inflammatory disease. N Engl J Med 1999; 340: 115-26.
- Chaldakov G, Fiore M, Ghenev P, et al. Atherosclerotic lesions: possible interactive involvement of intima, adventitia and associated adipose tissue. Int Med J 2000; 7: 43-9.
- Chaldakov G, Stankulov IS and Aloe L. Subepicardial adipose tissue in human coronary atherosclerosis: another neglected phenomenon. Atherosclerosis 2001; 154: 237-8.
- Gollasch M and Dubrovska G. Paracrine role for periadventitial adipose tissue in the regulation of arterial tone. Trends Pharmacol Sci 2004; 25: 647-53.
- Yudkin JS, Eringa E and Stehouwer CD. "Vasocrine" signalling from perivascular fat: a mechanism linking insulin resistance to vascular disease. Lancet 2005; 365: 1817-20.
- Takaoka M, Nagata D, Kihara S, et al. Periadventitial adipose tissue plays a critical role in vascular remodeling. Circ Res 2009; 105: 906-11.
- Lu C, Su LY, Lee RM, et al. Mechanisms for perivascular adipose tissue-mediated potentiation of vascular contraction to perivascular neuronal stimulation: the role of adipocyte-derived angiotensin II. Eur J Pharmacol 2010; 634: 107-12.
- Chaldakov G. Cardiovascular adipobiology: a novel. Heart-associated adipose tissue in cardiovascular disease. Ser J Exp Clin Res 2008; 9: 81-8.
- Ding J, Hsu FC, Harris TB, et al. The association of pericardial fat with incident coronary heart disease: the Multi-Ethnic Study of Atherosclerosis (MESA). Am J Clin Nutr 2009; 90: 499-504.
- Brinkley TE, Hsu FC, Carr JJ, et al. Pericardial fat is associated with carotid stiffness in the Multi-Ethnic Study of Atherosclerosis. Nutr Metab Cardiovasc Dis 2010.
- Karastergiou K, Evans I, Ogston N, et al. Epicardial adipokines in obesity and coronary artery disease induce atherogenic changes in monocytes and endothelial cells. Arterioscler Thromb Vasc Biol 2010; 30: 1340-6.
- Schlett CL, Massaro JM, Lehman SJ, et al. Novel measurements of periaortic adipose tissue in comparison to anthropometric measures of obesity, and abdominal adipose tissue. Int J Obes (Lond) 2009; 33: 226-32.
- Skilton MR, Serusclat A, Sethu AH, et al. Noninvasive measurement of carotid extra-media thickness: associations with cardiovascular risk factors and intima-media thickness. JACC Cardiovasc Imaging 2009; 2: 176-82.
- Thomas EL, Saeed N, Hajnal JV, et al. Magnetic resonance imaging of total body fat. J Appl Physiol 1998; 85: 1778-85.
- Chaldakov G, Tonchev AB and Aloe L. NGF and BDNF: from nerves to adipose tissue, from neurokines to metabokines. Riv Psichiatr 2009; 44: 79-87.
- Frisardi V, Solfrizzi V, Seripa D, et al. Metabolic-cognitive syndrome: a cross-talk between metabolic syndrome and Alzheimer's disease. Ageing Res Rev 2010; 9: 399-417.
Download this article (PDF version, 1.1 Mb) Download this issue (PDF version, 5.3 Mb)




