Abdominal Obesity and CVD
Defining CMR - Epidemiology - Abdominal Obesity vs. CVD: Beyond Body WeightKey Points
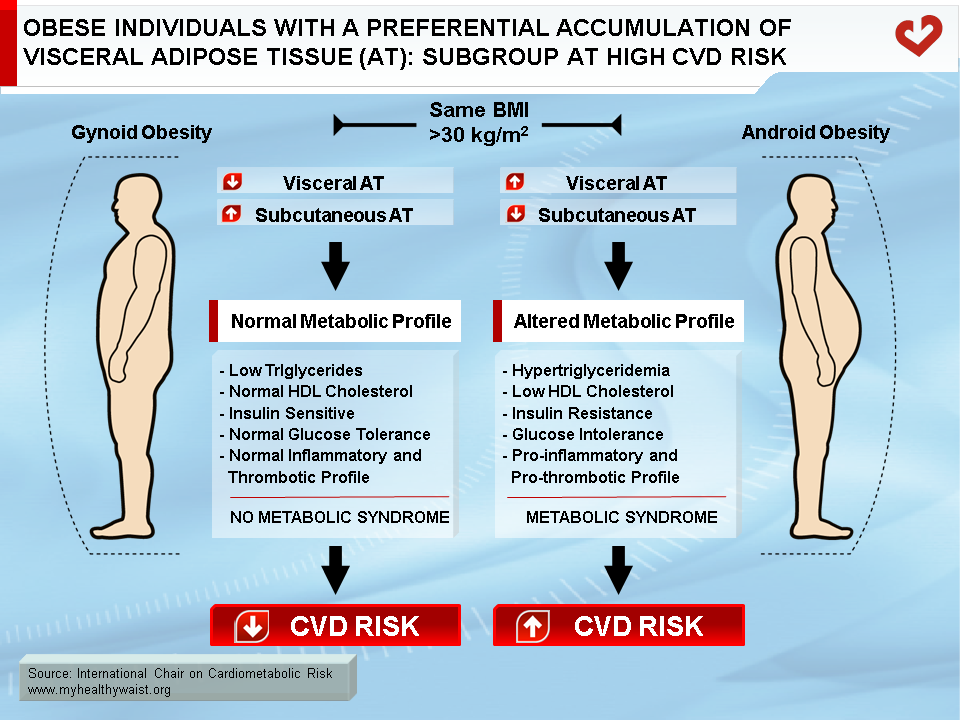
- Metabolic studies have shown that in both men and women the amount of visceral adipose tissue is strongly linked to metabolic abnormalities that increase the risk of type 2 diabetes and CVD.
- Overall obesity increases CVD risk. A wealth of data also indicates that obese individuals with high levels of abdominal fat—visceral fat in particular—form an obese subgroup with the worst metabolic profile.
- Because not every obese patient is at increased risk of CVD, the challenge for clinicians is to identify the subgroup of patients at highest risk of CVD. This requires clinicians to do more than measure body weight and calculate BMI.
- In order to properly evaluate CVD risk among overweight/obese patients, emphasis should be placed on estimating visceral adipose tissue using simple tools such as waist circumference.
Obesity: a Health Hazard
Most clinicians agree that obesity is a health hazard because of its ties to a host of metabolic complications such as dyslipidemia, type 2 diabetes, and cardiovascular disease (CVD) [1]. In today’s society, obesity is the driving force behind the rise in CVD [2]. The American Heart Association has singled out obesity as a major modifiable risk factor for heart disease [3,4]. Moreover, the Framingham Heart Study—a 26-year follow-up analysis conducted in men and women—revealed that body weight was independently related to development of CVD [5]. Additional studies have provided further evidence for a univariate relationship between obesity and CVD [6-10]. Although many epidemiological studies have linked body weight and coronary artery disease (CAD) [11-13], other studies using multivariate analysis have failed to identify obesity as an independent CVD risk factor [14,15]. In some cases, obesity’s contribution to CAD was no longer found to be significant after controlling for traditional CAD risk factors [6]. The exact relationship of CVD to body weight remains controversial and is still debated within the scientific community.
Heterogeneity of Obesity
The equivocal data on obesity and mortality may be explained by the fact that most epidemiological studies have used anthropometric correlates of total body fat (the most commonly used being body mass index—BMI—expressed in kg/m2) instead of taking into account the location of excess body fat, which seems to play a greater role in obesity-related health hazards. However, indices of overall obesity do not take into account the remarkable heterogeneity among overweight/obese patients [16]. In this regard, physicians are constantly challenged by the absence of metabolic complications in some very obese patients with a relatively “normal” metabolic profile despite their obvious excess body fat. Conversely, slightly overweight patients can display a cluster of atherogenic metabolic abnormalities that increase their risk of CVD. This variation in body fat distribution among obese patients was first noted by French physician Jean Vague in the mid-forties [17]. He reported that the complications generally found in obese patients depended more on the location of the excess fat rather than on obesity per se [17]. Vague used the term “android obesity” to describe the high-risk form of obesity, which is characterized by an accumulation of adipose tissue in the trunk and is commonly found in men. He described the accumulation of body fat in the gluteo-femoral region—the common fat pattern of premenopausal women—as “gynoid obesity.” This type of obesity is rarely associated with the common complications of excess adiposity [18,19]. However, it took the medical community some time to realize the significance of Vague’s clinical observations about sex differences in body fat distribution. The concept of regional adipose tissue distribution only received serious consideration in the 1980s, when prospective studies also showed that abdominal fat was associated with mortality, independent of total adiposity as estimated by BMI [20-22]. These studies provided sound evidence that regional fat distribution—as evaluated by anthropometric indices such as waist circumference and trunk skinfolds—was tied to increased CVD risk [20,21,23].
BMI: a Weak Correlate of Metabolic Syndrome Abnormalities
According to international guidelines, obesity is defined as a BMI of 30 kg/m2 or more [24]. BMI is commonly used as a valuable index of relative body weight and a crude estimate of total adiposity [25]. Although of great use in estimating overall obesity, this clinical tool has serious limitations. First, the index assumes that weight is distributed evenly over the body [1] and does not take into account the heterogeneity of obesity [16]. For example, individuals with large muscle mass but without excess body fat (e.g., American football and ice hockey or rugby players) could be misclassified as having a high-risk body weight. In addition, BMI does not provide information on body fat location, which has been shown to be a critical correlate of metabolic disturbances leading to CVD [26]. In this regard, several studies relating BMI to CVD outcomes in healthy individuals have reported inconsistent results. Some studies have found a linear relationship between BMI and cardiovascular risk, whereas others have failed to find an association [20,21,27-29]. However, most studies on the issue have not measured abdominal adiposity. In the Heart Outcomes Prevention Evaluation (HOPE) prospective study conducted in men and women with stable CVD, Dagenais et al. [30] found that BMI was no longer an independent predictor of myocardial infarction after adjusting for abdominal obesity indices such as waist-to-hip ratio (WHR) and waist circumference. Moreover, after adjusting for traditional risk factors such as BMI, waist circumference and WHR were independent predictors of CVD death, myocardial infarction, and total mortality [30]. Other studies carried out in subjects without known CVD have also reported that WHR and waist circumference were better predictors of coronary heart disease than BMI [20,31]. For example, a 13-year follow-up study of 792 men reported that a high WHR increased ischemic heart disease risk while indices of total obesity had no predictive value [21]. The authors concluded that although the association between WHR and CVD risk was not significant in multivariate analyses when cholesterol levels and blood pressure were taken into account, WHR was more closely related to CVD risk than other indices of obesity such as skinfold thickness or BMI [21]. An additional prospective study conducted in women also reported similar findings [20].
This latter study examined whether an android phenotype—the high-risk form of abdominal obesity commonly found in men—also increased CVD risk in women. Over a 12-year follow-up, the authors found that WHR was a better predictor of myocardial infarction in women than other indices of total adiposity. Accordingly, the study concluded that women with a typically masculine distribution of adipose tissue could represent a subgroup at high risk of CVD.
In the Nurses’ Health Study [32]—a follow-up study conducted on a cohort of more than 44,000 women free of coronary heart disease (CHD) at baseline—Rexrode et al. examined the 8-year incidence of CHD among tertiles of baseline BMI and waist circumference values. They found that both elevated WHR and waist circumference were independently associated with a twofold increase in CHD risk, even after adjusting for hypertension, diabetes, and high cholesterol. They also reported that higher waist circumference values increased CHD risk, regardless of BMI tertile. In addition, they found that the CHD risk of overweight/obese women (BMI>25.2 kg/m2) who were not abdominally obese (waist circumference <73.7 cm) was similar to the CHD risk of non-obese women (BMI <22.2 kg/m2) with higher levels of abdominal fat (waist circumference >81.8 cm). These findings highlight the need to go beyond body weight and BMI and take into account adipose tissue distribution in evaluating CHD risk.
A large myocardial infarction cases/controls study—INTERHEART [33]—was conducted in a sample of 27,098 participants from 52 countries. The study showed that WHR and waist circumference were closely tied to risk of myocardial infarction even after adjusting for other risk factors. The risk of myocardial infarction not only rose progressively with increasing WHR values, it also increased in each BMI category, suggesting that WHR is a good predictor of myocardial infarction in lean (BMI<25 kg/m2), overweight (BMI>25 kg/m2), and obese individuals (BMI>30 kg/m2). The authors concluded that WHR was a stronger anthropometric correlate of myocardial infarction and could be significantly better than BMI in assessing the risk of myocardial infarction in the general population.
Moreover, a prospective case-control study by Kuk et al. [34] examined 192 men (97 decedents and 194 controls) to establish whether abdominal fat was independently linked to mortality. The study revealed that visceral adipose tissue was a strong independent predictor of all-cause mortality in men. These findings could suggest that visceral fat should become a target of strategies to reduce obesity-related mortality and morbidity. Measuring waist circumference—which is the best anthropometric parameter for evaluating the absolute amount of abdominal visceral fat—therefore facilitates the identification of patients with visceral obesity, insulin resistance, and metabolic complications increasing the risk of CVD [35]. Although common indices of overall adiposity have been shown to predict CVD in both men and women, visceral fat accumulation appears to be the crucial factor tying obesity to CVD.
In order to highlight the limitations of BMI, 40 years ago Ruderman et al. [36,37] introduced the concept of the metabolically obese, normal weight (MONW) subject. These MONW individuals, who have normal BMI values, nonetheless suffer from metabolic complications commonly found in obese people. MONW individuals display a constellation of risk factors such as insulin resistance, abdominal adiposity, low HDL cholesterol levels, elevated triglycerides, impaired fasting glucose, and hypertension. Together these risk factors are also known as the metabolic syndrome [38]. Conversely, metabolically healthy obese (MHO) individuals described by other research groups have a BMI above 30 kg/m2 but are not characterized by features of insulin resistance [39,40]. Initially described by Jean Vague, these two phenotypes illustrate obesity’s remarkable heterogeneity when estimated using BMI as well as this index’s limitations in clinical practice. As demonstrated by Meigs et al. [41], subgroups of overweight or obese individuals have a heterogeneous metabolic risk profile. For instance, the authors observed that some normal weight men and women had features of the metabolic syndrome or insulin resistance, whereas some obese individuals had no metabolic abnormalities despite their significant obesity.
The notion of normal weight, metabolically obese subjects has also been documented by St-Onge et al. [42], who quantified the metabolic syndrome’s prevalence among normal weight and slightly overweight individuals. In this report, subjects in the upper (23.0-24.5 kg/m2) and just above normal BMI range (25.0-26.9 kg/m2)—also referred to as MONW individuals—were more likely to have the metabolic syndrome than individuals with a BMI below 20.9 kg/m2. These results suggest that CVD risk may increase far below the normal BMI cutoff of 25 kg/m2.
Given the crucial role played by visceral adiposity in the metabolic abnormalities of overweight and obesity, a key factor underpinning the difference in CVD risk between MONW and MHO individuals is likely the presence of excess visceral adipose tissue, which has been shown to increase CVD risk [43-45]. Most MONW individuals with relatively low BMI likely have a significant amount of visceral fat, and most MHO individuals with a high BMI likely have much less visceral adipose tissue [46]. Similarly, Matsuzawa et al. [47] have demonstrated that very obese individuals with a small amount of visceral adipose tissue—active sumo wrestlers, for example—are quite insulin sensitive, whereas retired sedentary sumo wrestlers with greater amounts of visceral adipose tissue tend to be insulin resistant and have a high prevalence of metabolic complications such as type 2 diabetes and CVD. These observations lend weight to the notion that visceral adipose tissue is the key factor behind the metabolic complications found in MONW individuals and strongly suggest that we need to look further than BMI, which is a weak correlate of the metabolic syndrome.
Body Fat Distribution: The Importance of Visceral Adipose Tissue
Fujioka et al. [43] were the first to propose that a preferential accumulation of visceral adipose tissue could explain the deterioration in glucose and lipid metabolism observed in obese patients. In their study, subjects with a preferential accumulation of visceral adipose tissue had higher fasting plasma triglyceride levels and higher plasma glucose responses following an oral glucose tolerance test (OGTT) than subjects with the same BMI values but a preferential accumulation of abdominal subcutaneous adipose tissue. The independent contribution of visceral adipose tissue vs. subcutaneous adipose tissue has also been examined in obese individuals with similar BMI values but either low or high amounts of visceral adipose tissue [48,49]. While obese subjects with low levels of visceral adipose tissue had a basically normal plasma lipoprotein-lipid profile, the subgroup of obese individuals with elevated visceral fat had the worst metabolic profile: fasting hypertriglyceridemia, low HDL cholesterol concentrations, glucose intolerance, hyperinsulinemia, and a prothrombotic and inflammatory state. Additional studies by Ross et al. [50,51] further explored the relationship between visceral adipose tissue and metabolic risk in men and women. When individuals who were matched for similar abdominal subcutaneous adipose tissue but had different levels of visceral adipose tissue were compared, it was revealed that subjects with high visceral adipose tissue had higher glucose values following an OGTT and lower glucose disposal values compared to subjects with low visceral adipose tissue. This means that obese individuals with a preferential accumulation of visceral adipose tissue may form an obese subgroup at highest risk of CVD. These findings indicate that overall obesity is associated with moderate metabolic complications, but that excess visceral adipose tissue is associated with a cluster of metabolic abnormalities that increase CVD risk. Therefore, for the same amount of total body fat, individuals with more visceral adipose tissue are at significantly greater risk of also having features of the metabolic syndrome [48-52].
In summary, there is a wealth of evidence indicating that obesity is a major modifiable risk factor for heart disease. However, obesity is a heterogeneous condition, and not every obese individual is at high risk of CVD. In this regard, several studies have shown that abdominal obesity could be a stronger predictor of CVD than overall obesity. Excess visceral adipose tissue is therefore linked to a pro-atherogenic and pro-diabetic profile that increases CVD risk (Figure). A joint position statement from the International Atherosclerosis Society and the International Chair on Cardiometabolic Risk Working Group on Visceral Obesity summarises the evidence for visceral adiposity and ectopic fat as emerging risk factors for type 2 diabetes, atherosclerosis, and CVD [53].
References
-
Bray GA, Bouchard C and James WPT, eds. Handbook of obesity. New York: Marcel Dekker. 1998.
PubMed ID:
-
Poirier P and Després JP. Waist circumference, visceral obesity, and cardiovascular risk. J Cardiopulm Rehabil 2003; 23: 161-9.
PubMed ID: 12782898
-
Eckel RH. Obesity and heart disease: a statement for healthcare professionals from the Nutrition Committee, American Heart Association. Circulation 1997; 96: 3248-50.
PubMed ID: 9386201
-
Eckel RH and Krauss RM. American Heart Association call to action: obesity as a major risk factor for coronary heart disease. AHA Nutrition Committee. Circulation 1998; 97: 2099-100.
PubMed ID: 9626167
-
Hubert HB, Feinleib M, McNamara PM, et al. Obesity as an independent risk factor for cardiovascular disease: a 26- year follow-up of participants in the Framingham Heart Study. Circulation 1983; 67: 968-77.
PubMed ID: 6219830
-
Keys A, Aravanis C, Blackburn H, et al. Coronary heart disease: overweight and obesity as risk factors. Ann Intern Med 1972; 77: 15-27.
PubMed ID: 5052445
-
Manson JE, Colditz GA, Stampfer MJ, et al. A prospective study of obesity and risk of coronary heart disease in women. N Engl J Med 1990; 322: 882-9.
PubMed ID: 2314422
-
Reed D and Yano K. Predictors of arteriographically defined coronary stenosis in the Honolulu Heart Program. Comparisons of cohort and arteriography series analyses. Am J Epidemiol 1991; 134: 111-22.
PubMed ID: 1862795
-
Freedman DS, Williamson DF, Croft JB, et al. Relation of body fat distribution to ischemic heart disease. The National Health and Nutrition Examination Survey I (NHANES I) Epidemiologic Follow-up Study. Am J Epidemiol 1995; 142: 53-63.
PubMed ID: 7785674
-
Fitzgerald AP and Jarrett RJ. Body weight and coronary heart disease mortality: an analysis in relation to age and smoking habit. 15 years follow-up data from the Whitehall Study. Int J Obes Relat Metab Disord 1992; 16: 119-23.
PubMed ID: 1316326
-
Barrett-Connor EL. Obesity, atherosclerosis, and coronary artery disease. Ann Intern Med 1985; 103: 1010-9.
PubMed ID: 3904565
-
Duflou J, Virmani R, Rabin I, et al. Sudden death as a result of heart disease in morbid obesity. Am Heart J 1995; 130: 306-13.
PubMed ID: 7631612
-
Bharati S and Lev M. Cardiac conduction system involvement in sudden death of obese young people. Am Heart J 1995; 129: 273-81.
PubMed ID: 7832099
-
Relationship of blood pressure, serum cholesterol, smoking habit, relative weight and ECG abnormalities to incidence of major coronary events: final report of the pooling project. The pooling project research group. J Chronic Dis 1978; 31: 201-306.
PubMed ID: 681498
-
Bray GA, Davidson MB and Drenick EJ. Obesity: a serious symptom. Ann Intern Med 1972; 77: 779-95.
PubMed ID: 4562970
-
Després JP, Lemieux I and Prud’homme D. Treatment of obesity: need to focus on high risk abdominally obese patients. BMJ 2001; 322: 716-20.
PubMed ID: 11264213
-
Vague J. La différenciation sexuelle: facteur déterminant des formes de l’obésité. Presse Med 1947; 339-40.
PubMed ID:
-
Terry RB, Stefanick ML, Haskell WL, et al. Contributions of regional adipose tissue depots tp plasma lipoprotein concentrations in overweight men and women: possible protective effects of thigh fat. Metabolism 1991; 40: 733-40.
PubMed ID: 1870428
-
Pouliot MC, Després JP, Nadeau A, et al. Associations between regional body fat distribution, fasting plasma free fatty acid levels and glucose tolerance in premenopausal women. Int J Obes 1990; 14: 293-302.
PubMed ID: 2361806
-
Lapidus L, Bengtsson C, Larsson BO, et al. Distribution of adipose tissue and risk of cardiovascular disease and death: a 12 year follow up of participants in the population study of women in Gothenburg, Sweaden. BMJ 1984; 289: 1261-3.
PubMed ID: 6437507
-
Larsson B, Svardsudd K, Welin L, et al. Abdominal adipose tissue distribution, obesity, and risk of cardiovascular disease and death: 13 year follow up of participants in the study of men born in 1913. BMJ (Clin Res Ed) 1984; 288: 1401-4.
PubMed ID: 6426576
-
Donahue RP, Abbott RD, Bloom E, et al. Central obesity and coronary heart disease in men. Lancet 1987; 1: 821-4.
PubMed ID: 2882231
-
Ducimetiere P, Richard J and Cambien F. The pattern of subcutaneous fat distribution in middle-aged men and the risk of coronary heart disease: the Paris Prospective Study. Int J Obes 1986; 10: 229-40.
PubMed ID: 3759330
-
Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults–The Evidence Report. National Institutes of Health. Obes Res 1998; 6 Suppl 2: 51S-209S.
PubMed ID: 9813653
-
Garrow J and Summerbell C. Meta-analysis on the effect of exercise on the composition of weight loss. Int J Obes Relat Metab Disord 1994; 18: 516-7.
PubMed ID: 7920879
-
Kissebah AH, Freedman DS and Peiris AN. Health risks of obesity. Med Clin North Am 1989; 73: 111-38.
PubMed ID: 2643000
-
Wilson PW, D’Agostino RB, Sullivan L, et al. Overweight and obesity as determinants of cardiovascular risk: the Framingham experience. Arch Intern Med 2002; 162: 1867-72.
PubMed ID: 12196085
-
Wannamethee SG, Shaper AG, Walker M, et al. Lifestyle and 15-year survival free of heart attack, stroke, and diabetes in middle-aged British men. Arch Intern Med 1998; 158: 2433-40.
PubMed ID: 9855381
-
Stevens J, Cai J, Pamuk ER, et al. The effect of age on the association between body-mass index and mortality. N Engl J Med 1998; 338: 1-7.
PubMed ID: 9414324
-
Dagenais GR, Yi Q, Mann JF, et al. Prognostic impact of body weight and abdominal obesity in women and men with cardiovascular disease. Am Heart J 2005; 149: 54-60.
PubMed ID: 15660034
-
Folsom AR, Stevens J, Schreiner PJ, et al. Body mass index, waist/hip ratio, and coronary heart disease incidence in African Americans and whites. Atherosclerosis Risk in Communities Study Investigators. Am J Epidemiol 1998; 148: 1187-94.
PubMed ID: 9867265
-
Rexrode KM, Carey VJ, Hennekens CH, et al. Abdominal adiposity and coronary heart disease in women. JAMA 1998; 280: 1843-8.
PubMed ID: 9846779
-
Yusuf S, Hawken S, Ounpuu S, et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet 2005; 366: 1640-9.
PubMed ID: 16271645
-
Kuk JL, Katzmarzyk PT, Nichaman MZ, et al. Visceral fat is an independent predictor of all-cause mortality in men. Obesity (Silver Spring) 2006; 14: 336-41.
PubMed ID: 16571861
-
Lemieux I, Pascot A, Couillard C, et al. Hypertriglyceridemic waist: A marker of the atherogenic metabolic triad (hyperinsulinemia; hyperapolipoprotein B; small, dense LDL) in men? Circulation 2000; 102: 179-84.
PubMed ID: 10889128
-
Ruderman NB, Schneider SH and Berchtold P. The “metabolically-obese,” normal-weight individual. Am J Clin Nutr 1981; 34: 1617-21.
PubMed ID: 7270486
-
Ruderman NB, Berchtold P and Schneider S. Obesity-associated disorders in normal-weight individuals: some speculations. Int J Obes 1982; 6 Suppl 1: 151-7.
PubMed ID: 6749721
-
Grundy SM, Brewer HB, Jr., Cleeman JI, et al. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation 2004; 109: 433-8.
PubMed ID: 14744958
-
Ferrannini E, Natali A, Bell P, et al. Insulin resistance and hypersecretion in obesity. European Group for the Study of Insulin Resistance (EGIR). J Clin Invest 1997; 100: 1166-73.
PubMed ID: 9303923
-
Bonora E, Kiechl S, Willeit J, et al. Prevalence of insulin resistance in metabolic disorders: the Bruneck Study. Diabetes 1998; 47: 1643-9.
PubMed ID: 9753305
-
Meigs JB, Wilson PW, Fox CS, et al. Body mass index, metabolic syndrome, and risk of type 2 diabetes or cardiovascular disease. J Clin Endocrinol Metab 2006; 91: 2906-12.
PubMed ID: 16735483
-
St-Onge MP, Janssen I and Heymsfield SB. Metabolic syndrome in normal-weight Americans: new definition of the metabolically obese, normal-weight individual. Diabetes Care 2004; 27: 2222-8.
PubMed ID: 15333488
-
Fujioka S, Matsuzawa Y, Tokunaga K, et al. Contribution of intra-abdominal fat accumulation to the impairment of glucose and lipid metabolism in human obesity. Metabolism 1987; 36: 54-9.
PubMed ID: 3796297
-
Després JP, Nadeau A, Tremblay A, et al. Role of deep abdominal fat in the association between regional adipose tissue distribution and glucose tolerance in obese women. Diabetes 1989; 38: 304-9.
PubMed ID: 2645187
-
Sparrow D, Borkan GA, Gerzof SG, et al. Relationship of fat distribution to glucose tolerance Results of computed tomography in male participants of the Normative Aging Study. Diabetes 1986; 35: 411-5.
PubMed ID: 3956878
-
Ruderman N, Chisholm D, Pi-Sunyer X, et al. The metabolically obese, normal-weight individual revisited. Diabetes 1998; 47: 699-713.
PubMed ID: 9588440
-
Matsuzawa Y. Pathophysiology and molecular mechanisms of visceral fat syndrome: the Japanese experience. Diabetes Metab Rev 1997; 13: 3-13.
PubMed ID: 9134345
-
Després JP, Moorjani S, Lupien PJ, et al. Regional distribution of body fat, plasma lipoproteins, and cardiovascular disease. Arteriosclerosis 1990; 10: 497-511.
PubMed ID: 2196040
-
Pouliot MC, Després JP, Nadeau A, et al. Visceral obesity in men. Associations with glucose tolerance, plasma insulin, and lipoprotein levels. Diabetes 1992; 41: 826-34.
PubMed ID: 1612197
-
Ross R, Freeman J, Hudson R, et al. Abdominal obesity, muscle composition, and insulin resistance in premenopausal women. J Clin Endocrinol Metab 2002; 87: 5044-51.
PubMed ID: 12414870
-
Ross R, Aru J, Freeman J, et al. Abdominal adiposity and insulin resistance in obese men. Am J Physiol Endocrinol Metab 2002; 282: E657-63.
PubMed ID: 11832370
-
Després JP. Is visceral obesity the cause of the metabolic syndrome? Ann Med 2006; 38: 52-63.
PubMed ID: 16448989
-
Neeland IJ, Ross, R, Després JP, et al. Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement. Lancet Diabetes Endocrinol 2019; 7: 715-25.
PubMed ID: 31301983
 CLOSE
CLOSE
 CLOSE
CLOSE
Poirier P and Després JP. Waist circumference, visceral obesity, and cardiovascular risk. J Cardiopulm Rehabil 2003; 23: 161-9.
PubMed ID: 12782898 CLOSE
CLOSE
Eckel RH. Obesity and heart disease: a statement for healthcare professionals from the Nutrition Committee, American Heart Association. Circulation 1997; 96: 3248-50.
PubMed ID: 9386201 CLOSE
CLOSE
Eckel RH and Krauss RM. American Heart Association call to action: obesity as a major risk factor for coronary heart disease. AHA Nutrition Committee. Circulation 1998; 97: 2099-100.
PubMed ID: 9626167 CLOSE
CLOSE
Hubert HB, Feinleib M, McNamara PM, et al. Obesity as an independent risk factor for cardiovascular disease: a 26- year follow-up of participants in the Framingham Heart Study. Circulation 1983; 67: 968-77.
PubMed ID: 6219830 CLOSE
CLOSE
Keys A, Aravanis C, Blackburn H, et al. Coronary heart disease: overweight and obesity as risk factors. Ann Intern Med 1972; 77: 15-27.
PubMed ID: 5052445 CLOSE
CLOSE
Manson JE, Colditz GA, Stampfer MJ, et al. A prospective study of obesity and risk of coronary heart disease in women. N Engl J Med 1990; 322: 882-9.
PubMed ID: 2314422 CLOSE
CLOSE
Reed D and Yano K. Predictors of arteriographically defined coronary stenosis in the Honolulu Heart Program. Comparisons of cohort and arteriography series analyses. Am J Epidemiol 1991; 134: 111-22.
PubMed ID: 1862795 CLOSE
CLOSE
Freedman DS, Williamson DF, Croft JB, et al. Relation of body fat distribution to ischemic heart disease. The National Health and Nutrition Examination Survey I (NHANES I) Epidemiologic Follow-up Study. Am J Epidemiol 1995; 142: 53-63.
PubMed ID: 7785674 CLOSE
CLOSE
Fitzgerald AP and Jarrett RJ. Body weight and coronary heart disease mortality: an analysis in relation to age and smoking habit. 15 years follow-up data from the Whitehall Study. Int J Obes Relat Metab Disord 1992; 16: 119-23.
PubMed ID: 1316326 CLOSE
CLOSE
Barrett-Connor EL. Obesity, atherosclerosis, and coronary artery disease. Ann Intern Med 1985; 103: 1010-9.
PubMed ID: 3904565 CLOSE
CLOSE
Duflou J, Virmani R, Rabin I, et al. Sudden death as a result of heart disease in morbid obesity. Am Heart J 1995; 130: 306-13.
PubMed ID: 7631612 CLOSE
CLOSE
Bharati S and Lev M. Cardiac conduction system involvement in sudden death of obese young people. Am Heart J 1995; 129: 273-81.
PubMed ID: 7832099 CLOSE
CLOSE
Relationship of blood pressure, serum cholesterol, smoking habit, relative weight and ECG abnormalities to incidence of major coronary events: final report of the pooling project. The pooling project research group. J Chronic Dis 1978; 31: 201-306.
PubMed ID: 681498 CLOSE
CLOSE
Bray GA, Davidson MB and Drenick EJ. Obesity: a serious symptom. Ann Intern Med 1972; 77: 779-95.
PubMed ID: 4562970 CLOSE
CLOSE
Després JP, Lemieux I and Prud’homme D. Treatment of obesity: need to focus on high risk abdominally obese patients. BMJ 2001; 322: 716-20.
PubMed ID: 11264213 CLOSE
CLOSE
 CLOSE
CLOSE
Terry RB, Stefanick ML, Haskell WL, et al. Contributions of regional adipose tissue depots tp plasma lipoprotein concentrations in overweight men and women: possible protective effects of thigh fat. Metabolism 1991; 40: 733-40.
PubMed ID: 1870428 CLOSE
CLOSE
Pouliot MC, Després JP, Nadeau A, et al. Associations between regional body fat distribution, fasting plasma free fatty acid levels and glucose tolerance in premenopausal women. Int J Obes 1990; 14: 293-302.
PubMed ID: 2361806 CLOSE
CLOSE
Lapidus L, Bengtsson C, Larsson BO, et al. Distribution of adipose tissue and risk of cardiovascular disease and death: a 12 year follow up of participants in the population study of women in Gothenburg, Sweaden. BMJ 1984; 289: 1261-3.
PubMed ID: 6437507 CLOSE
CLOSE
Larsson B, Svardsudd K, Welin L, et al. Abdominal adipose tissue distribution, obesity, and risk of cardiovascular disease and death: 13 year follow up of participants in the study of men born in 1913. BMJ (Clin Res Ed) 1984; 288: 1401-4.
PubMed ID: 6426576 CLOSE
CLOSE
Donahue RP, Abbott RD, Bloom E, et al. Central obesity and coronary heart disease in men. Lancet 1987; 1: 821-4.
PubMed ID: 2882231 CLOSE
CLOSE
Ducimetiere P, Richard J and Cambien F. The pattern of subcutaneous fat distribution in middle-aged men and the risk of coronary heart disease: the Paris Prospective Study. Int J Obes 1986; 10: 229-40.
PubMed ID: 3759330 CLOSE
CLOSE
Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults–The Evidence Report. National Institutes of Health. Obes Res 1998; 6 Suppl 2: 51S-209S.
PubMed ID: 9813653 CLOSE
CLOSE
Garrow J and Summerbell C. Meta-analysis on the effect of exercise on the composition of weight loss. Int J Obes Relat Metab Disord 1994; 18: 516-7.
PubMed ID: 7920879 CLOSE
CLOSE
Kissebah AH, Freedman DS and Peiris AN. Health risks of obesity. Med Clin North Am 1989; 73: 111-38.
PubMed ID: 2643000 CLOSE
CLOSE
Wilson PW, D’Agostino RB, Sullivan L, et al. Overweight and obesity as determinants of cardiovascular risk: the Framingham experience. Arch Intern Med 2002; 162: 1867-72.
PubMed ID: 12196085 CLOSE
CLOSE
Wannamethee SG, Shaper AG, Walker M, et al. Lifestyle and 15-year survival free of heart attack, stroke, and diabetes in middle-aged British men. Arch Intern Med 1998; 158: 2433-40.
PubMed ID: 9855381 CLOSE
CLOSE
Stevens J, Cai J, Pamuk ER, et al. The effect of age on the association between body-mass index and mortality. N Engl J Med 1998; 338: 1-7.
PubMed ID: 9414324 CLOSE
CLOSE
Dagenais GR, Yi Q, Mann JF, et al. Prognostic impact of body weight and abdominal obesity in women and men with cardiovascular disease. Am Heart J 2005; 149: 54-60.
PubMed ID: 15660034 CLOSE
CLOSE
Folsom AR, Stevens J, Schreiner PJ, et al. Body mass index, waist/hip ratio, and coronary heart disease incidence in African Americans and whites. Atherosclerosis Risk in Communities Study Investigators. Am J Epidemiol 1998; 148: 1187-94.
PubMed ID: 9867265 CLOSE
CLOSE
Rexrode KM, Carey VJ, Hennekens CH, et al. Abdominal adiposity and coronary heart disease in women. JAMA 1998; 280: 1843-8.
PubMed ID: 9846779 CLOSE
CLOSE
Yusuf S, Hawken S, Ounpuu S, et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet 2005; 366: 1640-9.
PubMed ID: 16271645 CLOSE
CLOSE
Kuk JL, Katzmarzyk PT, Nichaman MZ, et al. Visceral fat is an independent predictor of all-cause mortality in men. Obesity (Silver Spring) 2006; 14: 336-41.
PubMed ID: 16571861 CLOSE
CLOSE
Lemieux I, Pascot A, Couillard C, et al. Hypertriglyceridemic waist: A marker of the atherogenic metabolic triad (hyperinsulinemia; hyperapolipoprotein B; small, dense LDL) in men? Circulation 2000; 102: 179-84.
PubMed ID: 10889128 CLOSE
CLOSE
Ruderman NB, Schneider SH and Berchtold P. The “metabolically-obese,” normal-weight individual. Am J Clin Nutr 1981; 34: 1617-21.
PubMed ID: 7270486 CLOSE
CLOSE
Ruderman NB, Berchtold P and Schneider S. Obesity-associated disorders in normal-weight individuals: some speculations. Int J Obes 1982; 6 Suppl 1: 151-7.
PubMed ID: 6749721 CLOSE
CLOSE
Grundy SM, Brewer HB, Jr., Cleeman JI, et al. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation 2004; 109: 433-8.
PubMed ID: 14744958 CLOSE
CLOSE
Ferrannini E, Natali A, Bell P, et al. Insulin resistance and hypersecretion in obesity. European Group for the Study of Insulin Resistance (EGIR). J Clin Invest 1997; 100: 1166-73.
PubMed ID: 9303923 CLOSE
CLOSE
Bonora E, Kiechl S, Willeit J, et al. Prevalence of insulin resistance in metabolic disorders: the Bruneck Study. Diabetes 1998; 47: 1643-9.
PubMed ID: 9753305 CLOSE
CLOSE
Meigs JB, Wilson PW, Fox CS, et al. Body mass index, metabolic syndrome, and risk of type 2 diabetes or cardiovascular disease. J Clin Endocrinol Metab 2006; 91: 2906-12.
PubMed ID: 16735483 CLOSE
CLOSE
St-Onge MP, Janssen I and Heymsfield SB. Metabolic syndrome in normal-weight Americans: new definition of the metabolically obese, normal-weight individual. Diabetes Care 2004; 27: 2222-8.
PubMed ID: 15333488 CLOSE
CLOSE
Fujioka S, Matsuzawa Y, Tokunaga K, et al. Contribution of intra-abdominal fat accumulation to the impairment of glucose and lipid metabolism in human obesity. Metabolism 1987; 36: 54-9.
PubMed ID: 3796297 CLOSE
CLOSE
Després JP, Nadeau A, Tremblay A, et al. Role of deep abdominal fat in the association between regional adipose tissue distribution and glucose tolerance in obese women. Diabetes 1989; 38: 304-9.
PubMed ID: 2645187 CLOSE
CLOSE
Sparrow D, Borkan GA, Gerzof SG, et al. Relationship of fat distribution to glucose tolerance Results of computed tomography in male participants of the Normative Aging Study. Diabetes 1986; 35: 411-5.
PubMed ID: 3956878 CLOSE
CLOSE
Ruderman N, Chisholm D, Pi-Sunyer X, et al. The metabolically obese, normal-weight individual revisited. Diabetes 1998; 47: 699-713.
PubMed ID: 9588440 CLOSE
CLOSE
Matsuzawa Y. Pathophysiology and molecular mechanisms of visceral fat syndrome: the Japanese experience. Diabetes Metab Rev 1997; 13: 3-13.
PubMed ID: 9134345 CLOSE
CLOSE
Després JP, Moorjani S, Lupien PJ, et al. Regional distribution of body fat, plasma lipoproteins, and cardiovascular disease. Arteriosclerosis 1990; 10: 497-511.
PubMed ID: 2196040 CLOSE
CLOSE
Pouliot MC, Després JP, Nadeau A, et al. Visceral obesity in men. Associations with glucose tolerance, plasma insulin, and lipoprotein levels. Diabetes 1992; 41: 826-34.
PubMed ID: 1612197 CLOSE
CLOSE
Ross R, Freeman J, Hudson R, et al. Abdominal obesity, muscle composition, and insulin resistance in premenopausal women. J Clin Endocrinol Metab 2002; 87: 5044-51.
PubMed ID: 12414870 CLOSE
CLOSE
Ross R, Aru J, Freeman J, et al. Abdominal adiposity and insulin resistance in obese men. Am J Physiol Endocrinol Metab 2002; 282: E657-63.
PubMed ID: 11832370 CLOSE
CLOSE
Després JP. Is visceral obesity the cause of the metabolic syndrome? Ann Med 2006; 38: 52-63.
PubMed ID: 16448989 CLOSE
CLOSE
Neeland IJ, Ross, R, Després JP, et al. Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement. Lancet Diabetes Endocrinol 2019; 7: 715-25.
PubMed ID: 31301983