Respective Roles of Visceral Fat and Liver Fat
Defining CMR - Visceral Adipose Tissue: the Culprit? A Marker of Ectopic Fat Deposition?Key Points
- Visceral fat and liver fat are independently related to health risk. However, visceral fat is generally the stronger predictor of metabolic abnormalities, morbidity, and mortality.
- While the portal theory suggests that visceral fat and increased liver fat deposition are linked, the evidence for such a relationship is equivocal.
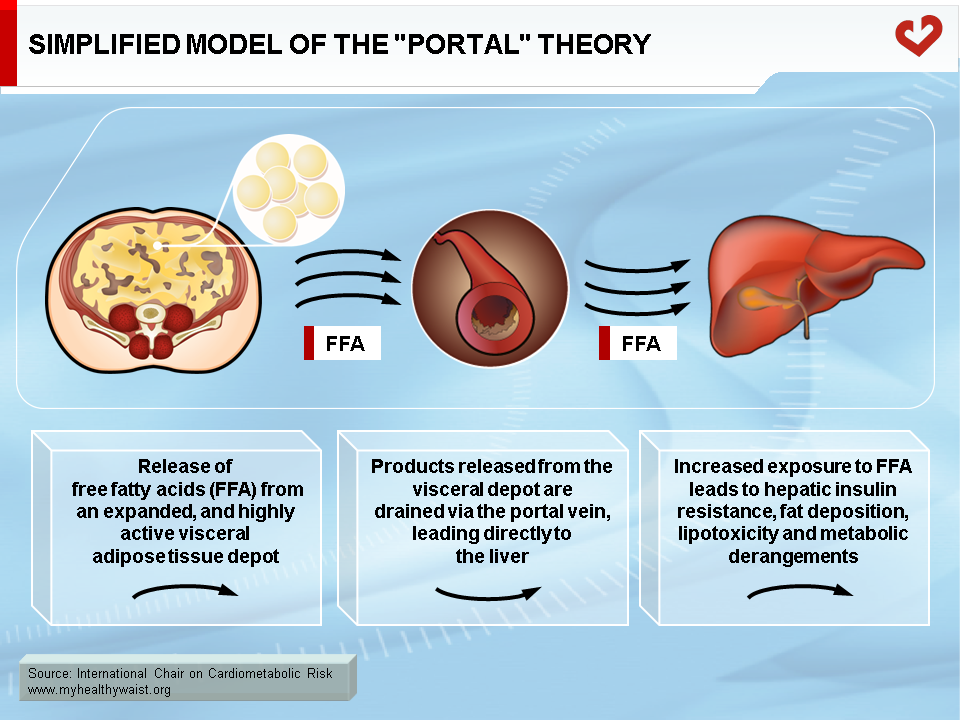
The Portal Theory
The portal theory links fatty liver to visceral fat [1]. Visceral fat is known to be both highly metabolically active [2] and to be drained by the portal vein [1], which connects to the liver. The portal theory suggests that high rates of lipolysis from the large visceral adipose depot cause excess free fatty acid (FFA) flux to the liver via the portal vein. This in turn leads to hepatic insulin resistance, triglyceride accumulation in the hepatocytes, and increased synthesis and secretion of atherogenic lipoproteins (see Liver Fat) (Figure 1). Supporting this theory is evidence of a moderate association between amount of visceral fat and degree of liver fat deposition [3-5]. Recent evidence also suggests that a high-fat diet increases lipid turnover from the visceral fat depot (due to enhanced gene expression of major regulators of FFA release). This may affect gene expression at the liver, causing more fat to be stored in hepatic tissue [6] and decreasing hepatic insulin clearance [7]. Further, it has been argued that the central nervous system may play a key role in the development of cardiometabolic risk and may link visceral adiposity to dysregulation of hepatic function [8]. Accordingly, it has been proposed that in a high-fat fed state, the adrenergic nervous system induces rhythmic lipolysis of visceral fat (which peaks during sleep), exposing the liver to excess FFA on an ongoing basis and possibly contributing to hepatic insulin resistance [8].
While some argue in favour of the portal theory or a link between visceral fat and liver fat [9], additional findings have failed to support this theory [10,11]. In addition, as scientific testing of the portal theory would require in vivo sampling of the portal vein, a difficult procedure, direct evidence supporting this hypothesis is hard to come by [12]. Moreover, new techniques have shown that of the FFA delivered to the liver via the portal vein, only approximately 5 to 20% of these come from visceral adipose tissue, with the remainder coming from the much larger subcutaneous fat depot [13]. The relationship between visceral fat and liver fat therefore remains largely theoretical and debatable [12].
Fatty Liver and Visceral Adipose Tissue
Although fatty liver is commonly associated with obesity [14], excess visceral fat in particular [3-5], many researchers have found that liver fat and metabolic complications are strongly linked, independent of total and abdominal obesity [4,5,11,15]. However, while both visceral fat and liver fat are clearly related to metabolic risk factors [5,16], exactly how these two fat depots are independently related to metabolic risk is difficult to detangle, and further evidence is needed. For example, several studies have reported that liver fat content is linked to metabolic risk independent of visceral adiposity in obese women with previous gestational diabetes [10], overweight non-diabetic men [11], and men with type 2 diabetes [17]. Conversely, other studies have reported that both visceral fat and liver fat independently predict certain metabolic risk factors [3,5]. However, in both studies the amount of visceral fat was the strongest predictor of metabolic abnormalities [3,5]. The amount of visceral adipose tissue, and not liver fat, has also been linked to selected metabolic risk factors in lean premenopausal women [18] and to all-cause mortality in a sample of men [19].
The degree of fat infiltration of the liver and the amount of visceral fat both seem to independently contribute to metabolic risk. While liver fat and visceral fat are clearly related, it has not yet been determined whether this relationship is causal or merely correlative. It is plausible that liver fat and visceral fat may simply be two depots for storing excess energy that develop independent of one another and increase metabolic risk via related or unrelated mechanisms (Figure 2).
References
-
Bjorntorp P. “Portal” adipose tissue as a generator of risk factors for cardiovascular disease and diabetes. Arteriosclerosis 1990; 10: 493-6.
PubMed ID: 2196039
-
Marin P, Andersson B, Ottosson M, et al. The morphology and metabolism of intraabdominal adipose tissue in men. Metabolism 1992; 41: 1242-8.
PubMed ID: 1435298
-
Kelley DE, McKolanis TM, Hegazi RA, et al. Fatty liver in type 2 diabetes mellitus: relation to regional adiposity, fatty acids, and insulin resistance. Am J Physiol Endocrinol Metab 2003; 285: E906-16.
PubMed ID: 12959938
-
Westerbacka J, Corner A, Tiikkainen M, et al. Women and men have similar amounts of liver and intra-abdominal fat, despite more subcutaneous fat in women: implications for sex differences in markers of cardiovascular risk. Diabetologia 2004; 47: 1360-9.
PubMed ID: 15309287
-
Nguyen-Duy TB, Nichaman MZ, Church TS, et al. Visceral fat and liver fat are independent predictors of metabolic risk factors in men. Am J Physiol Endocrinol Metab 2003; 284: E1065-71.
PubMed ID: 12554597
-
Kabir M, Catalano KJ, Ananthnarayan S, et al. Molecular evidence supporting the portal theory: a causative link between visceral adiposity and hepatic insulin resistance. Am J Physiol Endocrinol Metab 2005; 288: E454-61.
PubMed ID: 15522994
-
Kim SP, Ellmerer M, Van Citters GW, et al. Primacy of hepatic insulin resistance in the development of the metabolic syndrome induced by an isocaloric moderate-fat diet in the dog. Diabetes 2003; 52: 2453-60.
PubMed ID: 14514627
-
Bergman RN. Orchestration of glucose homeostasis: from a small acorn to the California oak. Diabetes 2007; 56: 1489-501.
PubMed ID: 17526912
-
Bergman RN, Kim SP, Catalano KJ, et al. Why visceral fat is bad: mechanisms of the metabolic syndrome. Obesity (Silver Spring) 2006; 14 Suppl 1: 16S-9S.
PubMed ID: 16642958
-
Tiikkainen M, Tamminen M, Hakkinen AM, et al. Liver-fat accumulation and insulin resistance in obese women with previous gestational diabetes. Obes Res 2002; 10: 859-67.
PubMed ID: 12226133
-
Seppala-Lindroos A, Vehkavaara S, Hakkinen AM, et al. Fat accumulation in the liver is associated with defects in insulin suppression of glucose production and serum free fatty acids independent of obesity in normal men. J Clin Endocrinol Metab 2002; 87: 3023-8.
PubMed ID: 12107194
-
Frayn KN. Visceral fat and insulin resistance–causative or correlative? Br J Nutr 2000; 83 Suppl 1: S71-7.
PubMed ID: 10889795
-
Klein S. The case of visceral fat: argument for the defense. J Clin Invest 2004; 113: 1530-2.
PubMed ID: 15173878
-
Dixon JB, Bhathal PS and O’Brien PE. Nonalcoholic fatty liver disease: predictors of nonalcoholic steatohepatitis and liver fibrosis in the severely obese. Gastroenterology 2001; 121: 91-100.
PubMed ID: 11438497
-
Marchesini G, Brizi M, Morselli-Labate AM, et al. Association of nonalcoholic fatty liver disease with insulin resistance. Am J Med 1999; 107: 450-5.
PubMed ID: 10569299
-
Banerji MA, Buckley MC, Chaiken RL, et al. Liver fat, serum triglycerides and visceral adipose tissue in insulin-sensitive and insulin-resistant black men with NIDDM. Int J Obes 1995; 19: 846-50.
PubMed ID: 8963350
-
Adiels M, Taskinen MR, Packard C, et al. Overproduction of large VLDL particles is driven by increased liver fat content in man. Diabetologia 2006; 49: 755-65.
PubMed ID: 16463046
-
Kuk JL, Nichaman MZ, Church TS, et al. Liver fat is not a marker of metabolic risk in lean premenopausal women. Metabolism 2004; 53: 1066-71.
PubMed ID: 16571861
-
Kuk JL, Katzmarzyk PT, Nichaman MZ, et al. Visceral fat is an independent predictor of all-cause mortality in men. Obesity (Silver Spring) 2006; 14: 336-41.
PubMed ID: 16571861
 CLOSE
CLOSE
Bjorntorp P. “Portal” adipose tissue as a generator of risk factors for cardiovascular disease and diabetes. Arteriosclerosis 1990; 10: 493-6.
PubMed ID: 2196039 CLOSE
CLOSE
Marin P, Andersson B, Ottosson M, et al. The morphology and metabolism of intraabdominal adipose tissue in men. Metabolism 1992; 41: 1242-8.
PubMed ID: 1435298 CLOSE
CLOSE
Kelley DE, McKolanis TM, Hegazi RA, et al. Fatty liver in type 2 diabetes mellitus: relation to regional adiposity, fatty acids, and insulin resistance. Am J Physiol Endocrinol Metab 2003; 285: E906-16.
PubMed ID: 12959938 CLOSE
CLOSE
Westerbacka J, Corner A, Tiikkainen M, et al. Women and men have similar amounts of liver and intra-abdominal fat, despite more subcutaneous fat in women: implications for sex differences in markers of cardiovascular risk. Diabetologia 2004; 47: 1360-9.
PubMed ID: 15309287 CLOSE
CLOSE
Nguyen-Duy TB, Nichaman MZ, Church TS, et al. Visceral fat and liver fat are independent predictors of metabolic risk factors in men. Am J Physiol Endocrinol Metab 2003; 284: E1065-71.
PubMed ID: 12554597 CLOSE
CLOSE
Kabir M, Catalano KJ, Ananthnarayan S, et al. Molecular evidence supporting the portal theory: a causative link between visceral adiposity and hepatic insulin resistance. Am J Physiol Endocrinol Metab 2005; 288: E454-61.
PubMed ID: 15522994 CLOSE
CLOSE
Kim SP, Ellmerer M, Van Citters GW, et al. Primacy of hepatic insulin resistance in the development of the metabolic syndrome induced by an isocaloric moderate-fat diet in the dog. Diabetes 2003; 52: 2453-60.
PubMed ID: 14514627 CLOSE
CLOSE
Bergman RN. Orchestration of glucose homeostasis: from a small acorn to the California oak. Diabetes 2007; 56: 1489-501.
PubMed ID: 17526912 CLOSE
CLOSE
Bergman RN, Kim SP, Catalano KJ, et al. Why visceral fat is bad: mechanisms of the metabolic syndrome. Obesity (Silver Spring) 2006; 14 Suppl 1: 16S-9S.
PubMed ID: 16642958 CLOSE
CLOSE
Tiikkainen M, Tamminen M, Hakkinen AM, et al. Liver-fat accumulation and insulin resistance in obese women with previous gestational diabetes. Obes Res 2002; 10: 859-67.
PubMed ID: 12226133 CLOSE
CLOSE
Seppala-Lindroos A, Vehkavaara S, Hakkinen AM, et al. Fat accumulation in the liver is associated with defects in insulin suppression of glucose production and serum free fatty acids independent of obesity in normal men. J Clin Endocrinol Metab 2002; 87: 3023-8.
PubMed ID: 12107194 CLOSE
CLOSE
Frayn KN. Visceral fat and insulin resistance–causative or correlative? Br J Nutr 2000; 83 Suppl 1: S71-7.
PubMed ID: 10889795 CLOSE
CLOSE
Klein S. The case of visceral fat: argument for the defense. J Clin Invest 2004; 113: 1530-2.
PubMed ID: 15173878 CLOSE
CLOSE
Dixon JB, Bhathal PS and O’Brien PE. Nonalcoholic fatty liver disease: predictors of nonalcoholic steatohepatitis and liver fibrosis in the severely obese. Gastroenterology 2001; 121: 91-100.
PubMed ID: 11438497 CLOSE
CLOSE
Marchesini G, Brizi M, Morselli-Labate AM, et al. Association of nonalcoholic fatty liver disease with insulin resistance. Am J Med 1999; 107: 450-5.
PubMed ID: 10569299 CLOSE
CLOSE
Banerji MA, Buckley MC, Chaiken RL, et al. Liver fat, serum triglycerides and visceral adipose tissue in insulin-sensitive and insulin-resistant black men with NIDDM. Int J Obes 1995; 19: 846-50.
PubMed ID: 8963350 CLOSE
CLOSE
Adiels M, Taskinen MR, Packard C, et al. Overproduction of large VLDL particles is driven by increased liver fat content in man. Diabetologia 2006; 49: 755-65.
PubMed ID: 16463046 CLOSE
CLOSE
Kuk JL, Nichaman MZ, Church TS, et al. Liver fat is not a marker of metabolic risk in lean premenopausal women. Metabolism 2004; 53: 1066-71.
PubMed ID: 16571861 CLOSE
CLOSE
Kuk JL, Katzmarzyk PT, Nichaman MZ, et al. Visceral fat is an independent predictor of all-cause mortality in men. Obesity (Silver Spring) 2006; 14: 336-41.
PubMed ID: 16571861