Hypertension
Defining CMR - Visceral Adipose Tissue: the Culprit? Complications of Visceral ObesityKey Points
- Hypertension is a well-known, potent, and modifiable CVD risk factor.
- Hypertension-related CVD risk escalates when other risk factors are present.
- Visceral obesity and hypertension are linked.
- The amount of visceral fat may explain the association between obesity, fasting insulin, insulin sensitivity, and blood pressure.
Hypertension and Cardiometabolic Risk
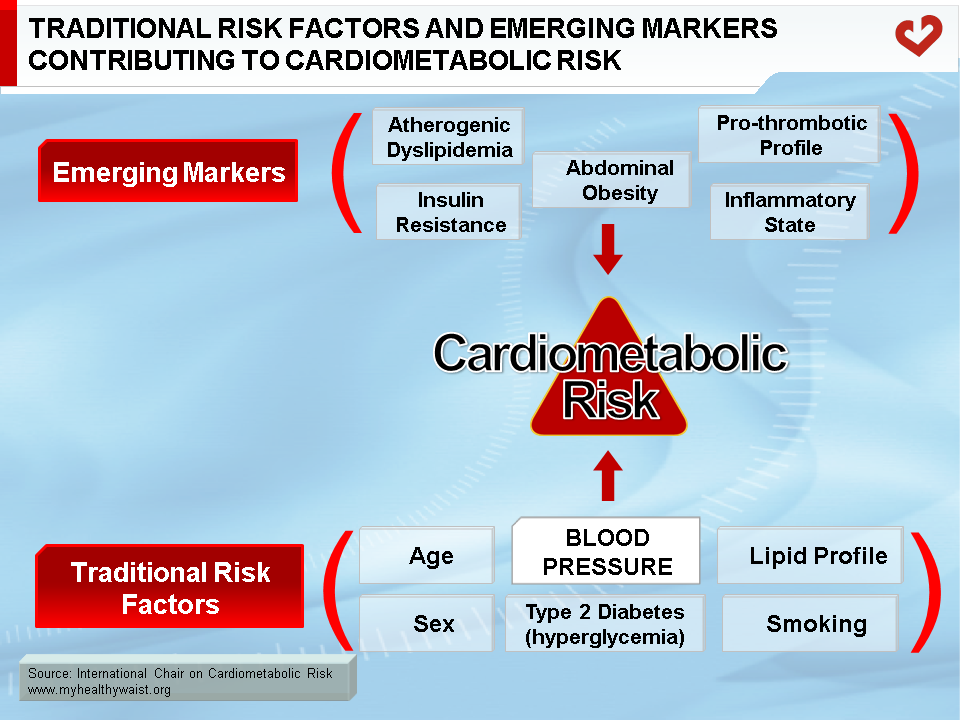
Cardiometabolic risk refers to an individual’s probability of developing type 2 diabetes and cardiovascular disease (CVD) due to the presence of “traditional” risk factors and emerging markers [1-3]. These risk factors include age, sex, blood pressure (BP), diabetes (hyperglycemia), smoking, LDL cholesterol, HDL cholesterol, and features of the metabolic syndrome. These features are most often found in individuals with overweight/obesity (particularly abdominal obesity), insulin resistance, atherogenic dyslipidemia, and a pro-thrombotic, inflammatory state [1,2]. As an indicator of global CVD risk, cardiometabolic risk includes traditional risk factors while taking into account the potential contribution of visceral obesity and/or insulin resistance and related metabolic markers (Figure 1) [1-3].
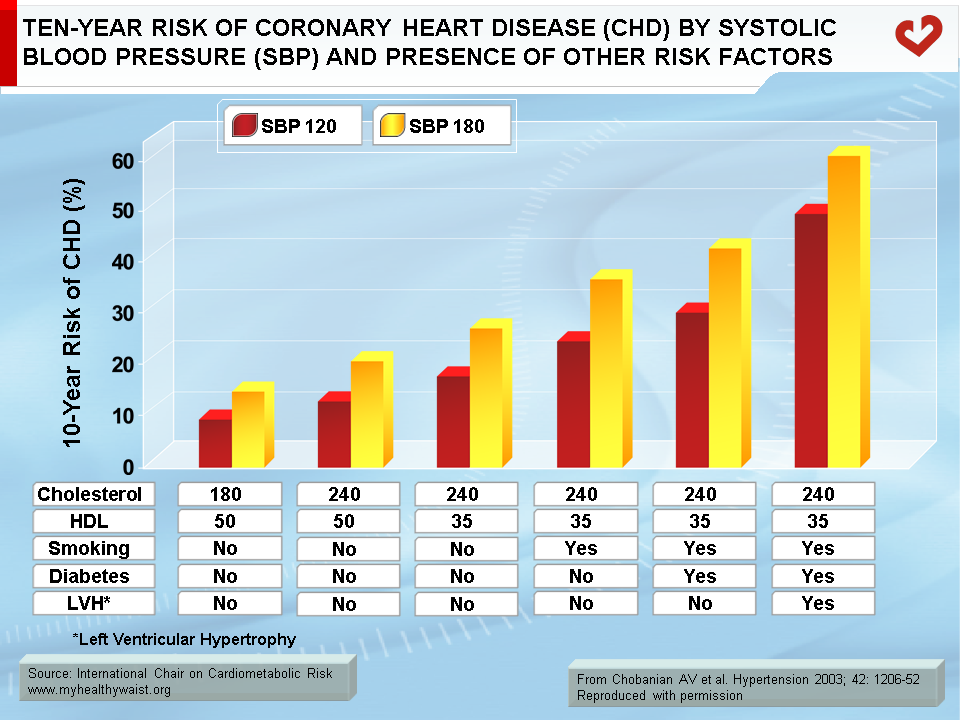
Hypertension is a potent and modifiable CVD risk factor [4,5]. The relationship between BP and CVD risk is linear, consistent, and independent of other risk factors. For instance, the probability of myocardial infarction, heart failure, chronic kidney disease, and stroke rises in step with BP [5]. From a start point of 115/75 mmHg, CVD risk doubles for each 20 mmHg rise in systolic BP and each 10 mmHg rise in diastolic BP [6]. Hypertension-related CVD risk also escalates in the presence of other risk factors [7] (Figure 2).
Definition
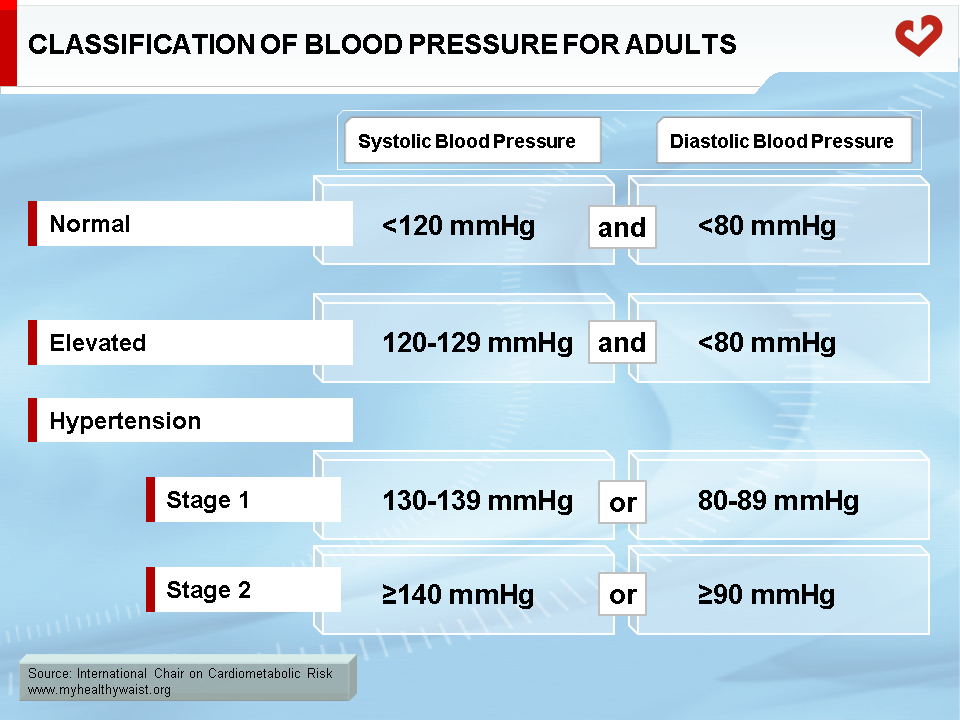
The classification of BP in adults is based on the average of 2 or more readings taken at each of 2 or more visits [8]. According to the last guidelines [5], BP classification for adults is indicated in the Table. To be considered with normal BP values, systolic BP must be <120 mmHg and diastolic BP must be <80 mmHg. Hypertension is diagnosed when systolic BP values are ≥130 mmHg or when diastolic BP ≥80 mmHg. When individuals have systolic BP values between 120-129 mmHg with normal diastolic BP values, they are classified as being in the elevated category. These patients are at risk of hypertension and CVD and making lifestyle changes is key for them to prevent an eventual progression to hypertension itself [5].
Hypertension may be essential (primary) or secondary. Secondary hypertension has an identifiable cause and accounts for 2% to 10% of cases. Essential hypertension is a diagnosis made in the absence of an identifiable secondary cause. Essential hypertension accounts for approximately 90% to 95% of hypertension cases [9].
Frequency and Impact of Gender and Age
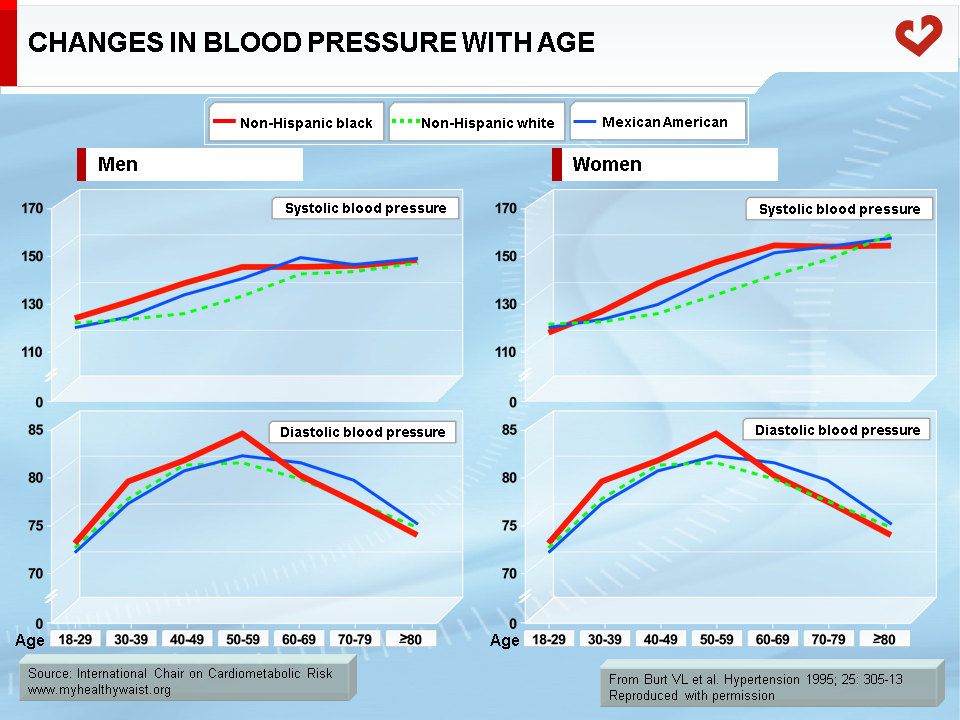
The age-adjusted prevalence of hypertension in the United States—defined by a systolic BP ≥130 mmHg and/or a diastolic BP ≥80 mmHg or patients taking antihypertensive medications—is 46% [5]. In Canadian adults, the prevalence of hypertension (systolic BP ≥140 mmHg and/or diastolic BP ≥90 mmHg or drug treatment) is 22.6% [10]. Of interest is the fact that ethnic origin has an impact on the prevalence of hypertension. Blacks have higher rates of hypertension compared to Caucasians [5]. BP also increases progressively with age (Figure 3) [5,11].
Blood Pressure Regulation and the Pathophysiology of Hypertension
Cardiac output and systemic vascular resistance modulate arterial BP. Accordingly, factors affecting both cardiac output and systemic vascular resistance influence arterial BP. Among the factors that influence cardiac output are sodium intake, renal function, and mineral corticoids [9]. Increased extracellular fluid volume, heart rate, and contractility also determine inotropic action. The sympathetic nervous system—via vasoconstriction and vasodilation—as well as humoral factors (angiotensin, catecholamines, prostaglandins, kinins, etc.) and local autoregulation all act on peripheral vascular resistance [9].
The exact cause of essential hypertension is not yet known. However, a mixture of adrenergic hyperactivity, genetic predisposition, altered calcium homeostasis, excess dietary salt intake, and alteration of the vascular endothelium are some likely contributors [9]. Compared to patients with hypertension alone, patients who are both hypertensive and obese have lower peripheral vascular resistance and higher cardiac output associated with an increased preload. Obesity-related hypertension also has a negative effect on renal function and is linked to an increased incidence of renal failure [12].
The Relationship Between Obesity and Hypertension
Hypertension triggers an array of cardiovascular damage, such as left ventricular hypertrophy, atrial and ventricular arrhythmias, diastolic heart failure, systolic heart failure, and ischemic heart disease with or without congestive heart failure [9]. Hypertension also harms the central nervous system and kidneys. The presence of other risk factors [7]—such as insulin resistance and the metabolic syndrome [1]—increases hypertension’s harmful impact on target organs and CVD risk.
Obesity has many damaging effects on physiological processes [1,13]. Obesity and hypertension are linked, with obese patients having higher rates of hypertension than normal-weight individuals [14,15]. Interestingly, not every obese patient is hypertensive, indicating that obesity is a heterogeneous condition [16]. Waist circumference has been reported as the strongest independent predictor of systolic BP and diastolic BP in normoglycemic Chinese [17]. Furthermore, excess visceral fat has been found to be associated with hypertension in Japanese Americans [18]. However, hypertension rates were rather high in both studies (56% and 25% respectively) [17,18]. Since some antihypertensive medications may influence insulin sensitivity and the metabolic risk profile over time, it is important to study the relationship of abdominal obesity and BP in population-based cohorts to avoid the influence of confounding factors [19].
In a population-based study—of which only 6.5% of subjects had hypertension—Poirier et al. [20] observed that waist circumference in men and women was most strongly linked to systolic BP and diastolic BP compared to other likely contributors such as insulin resistance and fasting insulin levels. The amount of visceral fat—crudely estimated as waist circumference—may therefore have largely explained the association between obesity, fasting insulin, insulin sensitivity, and BP [20].
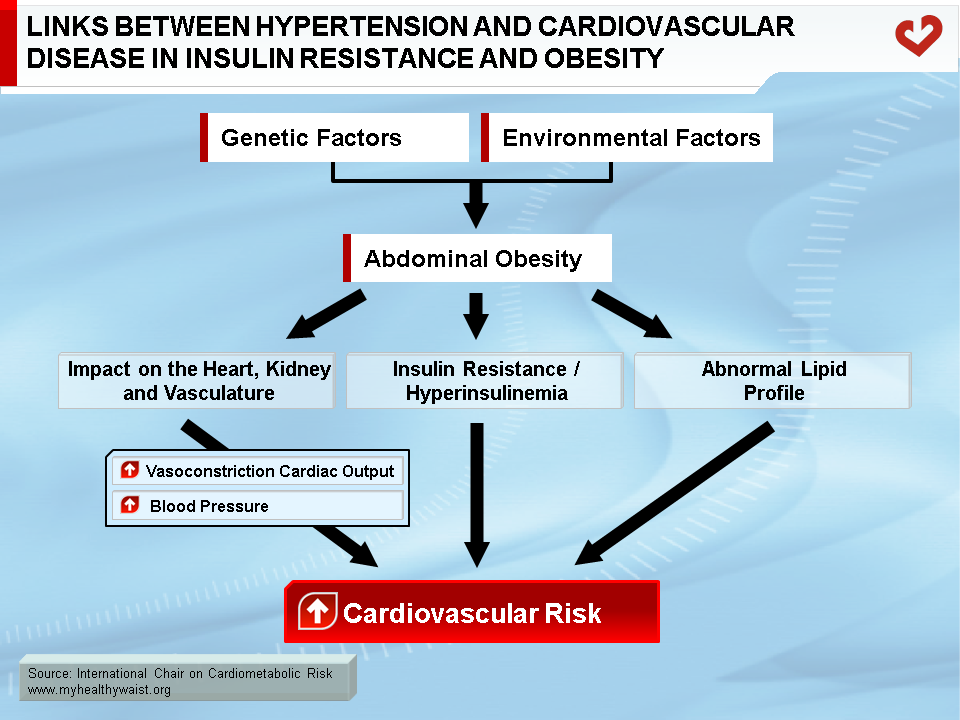
Which mechanisms underpin the elevated BP found with visceral obesity independent of insulin resistance? One possible answer lies in the formation of angiotensin II and aldosterone by obesity-induced sympathetic activation and the release of molecules by hypertrophied fat cells. A renin-angiotensin system has also been found in human adipose tissue. Obesity is also known to cause structural alterations in the kidneys that may eventually cause loss of nephron function and a further elevation in BP [21]. Figure 4 illustrates the putative mechanisms of hypertension and CVD in insulin resistance and obesity.
Obesity—abdominal obesity in particular—therefore seems to play an important role in the pathophysiology of hypertension and should not be neglected when determining therapeutic approaches to lowering BP.
References
-
Després JP and Lemieux I. Abdominal obesity and metabolic syndrome. Nature 2006; 444: 881-7.
PubMed ID: 17167477
-
Després JP, Lemieux I, Bergeron J, et al. Abdominal obesity and the metabolic syndrome: contribution to global cardiometabolic risk. Arterioscler Thromb Vasc Biol 2008; 28: 1039-49
PubMed ID: 18356555
-
Després JP, Cartier A, Côté M, et al. The concept of cardiometabolic risk: Bridging the fields of diabetology and cardiology. Ann Med 2008; 40: 514-23
PubMed ID: 18608131
-
G. B. D. Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018; 392: 1923-94
PubMed ID: 30496105
-
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Hypertension 2018; 71: e13-e115
PubMed ID: 29133356
-
Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360: 1903-13
PubMed ID: 12493255
-
Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42: 1206-52
PubMed ID: 14656957
-
Muntner P, Shimbo D, Carey RM, et al. Measurement of blood pressure in humans: a scientific statement from the American Heart Association. Hypertension 2019; 73: e35-e66
PubMed ID: 30827125
-
Alexander AR, Madhur MS, Harrison DG, et al. Hypertension. Medscape, February 22, 2019. https://emedicine.medscape.com/article/241381
PubMed ID:
-
Padwal RS, Bienek A, McAlister FA, et al. Epidemiology of hypertension in Canada: an update. Can J Cardiol 2016; 32: 687-94
PubMed ID: 26711315
-
Burt VL, Whelton P, Roccella EJ, et al. Prevalence of hypertension in the US adult population. Results from the Third National Health and Nutrition Examination Survey, 1988-1991. Hypertension 1995; 25: 305-13
PubMed ID: 7875754
-
Hall JE, do Carmo JM, da Silva AA, et al. Obesity, kidney dysfunction and hypertension: mechanistic links. Nat Rev Nephrol 2019; 15: 367-85
PubMed ID: 31015582
-
Poirier P, Giles TD, Bray GA, et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation 2006; 113: 898-918
PubMed ID: 16380542
-
Chiang BN, Perlman LV and Epstein FH. Overweight and hypertension. A review. Circulation 1969; 39: 403-21
PubMed ID: 4885946
-
Stamler R, Stamler J, Riedlinger WF, et al. Weight and blood pressure. Findings in hypertension screening of 1 million Americans. JAMA 1978; 240: 1607-10
PubMed ID: 691146
-
Poirier P and Després JP. Waist circumference, visceral obesity, and cardiovascular risk. J Cardiopulm Rehabil 2003; 23: 161-9
PubMed ID: 12782898
-
Thomas GN, Critchley JA, Tomlinson B, et al. Obesity, independent of insulin resistance, is a major determinant of blood pressure in normoglycemic Hong Kong Chinese. Metabolism 2000; 49: 1523-8
PubMed ID: 11145111
-
Hayashi T, Boyko EJ, Leonetti DL, et al. Visceral adiposity and the prevalence of hypertension in Japanese Americans. Circulation 2003; 108: 1718-23
PubMed ID: 12975250
-
Baba T and Neugebauer S. The link between insulin resistance and hypertension. Effects of antihypertensive and antihyperlipidaemic drugs on insulin sensitivity. Drugs 1994; 47: 383-404
PubMed ID: 7514971
-
Poirier P, Lemieux I, Mauriège P, et al. Impact of waist circumference on the relationship between blood pressure and insulin: the Quebec Health Survey. Hypertension 2005; 45: 363-7
PubMed ID: 15668356
-
Hall JE. The kidney, hypertension, and obesity. Hypertension 2003; 41: 625-33
PubMed ID: 12623970
 CLOSE
CLOSE
Després JP and Lemieux I. Abdominal obesity and metabolic syndrome. Nature 2006; 444: 881-7.
PubMed ID: 17167477 CLOSE
CLOSE
Després JP, Lemieux I, Bergeron J, et al. Abdominal obesity and the metabolic syndrome: contribution to global cardiometabolic risk. Arterioscler Thromb Vasc Biol 2008; 28: 1039-49
PubMed ID: 18356555 CLOSE
CLOSE
Després JP, Cartier A, Côté M, et al. The concept of cardiometabolic risk: Bridging the fields of diabetology and cardiology. Ann Med 2008; 40: 514-23
PubMed ID: 18608131 CLOSE
CLOSE
G. B. D. Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018; 392: 1923-94
PubMed ID: 30496105 CLOSE
CLOSE
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Hypertension 2018; 71: e13-e115
PubMed ID: 29133356 CLOSE
CLOSE
Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360: 1903-13
PubMed ID: 12493255 CLOSE
CLOSE
Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42: 1206-52
PubMed ID: 14656957 CLOSE
CLOSE
Muntner P, Shimbo D, Carey RM, et al. Measurement of blood pressure in humans: a scientific statement from the American Heart Association. Hypertension 2019; 73: e35-e66
PubMed ID: 30827125 CLOSE
CLOSE
Alexander AR, Madhur MS, Harrison DG, et al. Hypertension. Medscape, February 22, 2019. https://emedicine.medscape.com/article/241381
PubMed ID: CLOSE
CLOSE
Padwal RS, Bienek A, McAlister FA, et al. Epidemiology of hypertension in Canada: an update. Can J Cardiol 2016; 32: 687-94
PubMed ID: 26711315 CLOSE
CLOSE
Burt VL, Whelton P, Roccella EJ, et al. Prevalence of hypertension in the US adult population. Results from the Third National Health and Nutrition Examination Survey, 1988-1991. Hypertension 1995; 25: 305-13
PubMed ID: 7875754 CLOSE
CLOSE
Hall JE, do Carmo JM, da Silva AA, et al. Obesity, kidney dysfunction and hypertension: mechanistic links. Nat Rev Nephrol 2019; 15: 367-85
PubMed ID: 31015582 CLOSE
CLOSE
Poirier P, Giles TD, Bray GA, et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation 2006; 113: 898-918
PubMed ID: 16380542 CLOSE
CLOSE
Chiang BN, Perlman LV and Epstein FH. Overweight and hypertension. A review. Circulation 1969; 39: 403-21
PubMed ID: 4885946 CLOSE
CLOSE
Stamler R, Stamler J, Riedlinger WF, et al. Weight and blood pressure. Findings in hypertension screening of 1 million Americans. JAMA 1978; 240: 1607-10
PubMed ID: 691146 CLOSE
CLOSE
Poirier P and Després JP. Waist circumference, visceral obesity, and cardiovascular risk. J Cardiopulm Rehabil 2003; 23: 161-9
PubMed ID: 12782898 CLOSE
CLOSE
Thomas GN, Critchley JA, Tomlinson B, et al. Obesity, independent of insulin resistance, is a major determinant of blood pressure in normoglycemic Hong Kong Chinese. Metabolism 2000; 49: 1523-8
PubMed ID: 11145111 CLOSE
CLOSE
Hayashi T, Boyko EJ, Leonetti DL, et al. Visceral adiposity and the prevalence of hypertension in Japanese Americans. Circulation 2003; 108: 1718-23
PubMed ID: 12975250 CLOSE
CLOSE
Baba T and Neugebauer S. The link between insulin resistance and hypertension. Effects of antihypertensive and antihyperlipidaemic drugs on insulin sensitivity. Drugs 1994; 47: 383-404
PubMed ID: 7514971 CLOSE
CLOSE
Poirier P, Lemieux I, Mauriège P, et al. Impact of waist circumference on the relationship between blood pressure and insulin: the Quebec Health Survey. Hypertension 2005; 45: 363-7
PubMed ID: 15668356 CLOSE
CLOSE
Hall JE. The kidney, hypertension, and obesity. Hypertension 2003; 41: 625-33
PubMed ID: 12623970