NCEP-ATP III
Evaluating CMR - Metabolic Syndrome and Type 2 Diabetes/CVD RiskKey Points
- NCEP-ATP III guidelines have emphasized that the metabolic syndrome is a secondary target of therapy beyond elevated LDL cholesterol.
- NCEP-ATP III guidelines have also singled out excess abdominal adipose tissue as a key feature of the metabolic syndrome.
- Other elements of the metabolic syndrome include atherogenic dyslipidemia, insulin resistance, a pro-inflammatory and pro-thrombotic profile, and high blood pressure.
- To date, numerous prospective studies have shown that the metabolic syndrome predicts CVD risk, with very few exceptions.
- Overall CVD risk related to the metabolic syndrome has been evaluated in meta-analyses, which have concluded that the metabolic syndrome increases relative risk of CVD.
- The metabolic syndrome is a stronger predictor of type 2 diabetes than CVD risk.
The NCEP-ATP III Statement of 2001
The third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III or ATP III) was published in 2001 to provide updated guidelines for cholesterol testing and management [1,2]. The primary objective of this document was to demonstrate that patients with coronary heart disease (CHD) could benefit from intensive cholesterol-lowering treatment, while suggesting that special focus be placed on primary prevention in persons with multiple risk factors (other than elevated LDL cholesterol) in order to prevent CHD. These risk factors include traditional factors such as age, sex, total and HDL cholesterol, smoking, hypertension, family history of premature CHD, and diabetes without CHD. NCEP-ATP III was also the first to recognize the importance of the metabolic syndrome and identify it as a secondary target of risk-reduction therapy after the primary target, LDL cholesterol.
Several authors have proposed that abdominal obesity should be considered the underlying cause or, at least, the most prevalent form of the metabolic syndrome [3,4]. Linked to upper-body obesity, the metabolic syndrome is also associated with a cluster of metabolic abnormalities such as atherogenic dyslipidemia (elevated triglyceride and apolipoprotein B, low HDL cholesterol, and the presence of small, dense LDL and HDL particles), a pro-inflammatory and pro-thrombotic profile, insulin resistance, and elevated blood pressure. NCEP-ATP III sets out clinical criteria to help health professionals diagnose the metabolic syndrome in clinical practice.
These criteria are presented in Table. As outlined in the table, the metabolic syndrome is diagnosed if patients have three or more risk factors/markers, with the syndrome increasing CHD risk at any given LDL cholesterol level. However, these clinical tools are not a definition of the metabolic syndrome. NCEP-ATP III also recommends managing the metabolic syndrome for two reasons: to target the underlying causes of the metabolic syndrome (obesity and physical inactivity) and to treat nonlipid and lipid risk factors. Furthermore, NCEP-ATP III suggests that treatment of the metabolic syndrome should begin with lifestyle therapy aimed at achieving a healthy body weight.
Etiology and Treatment of the Metabolic Syndrome and its Components According to NCEP-ATP III (2005)
Some individuals and ethnic groups are genetically more prone to developing the metabolic syndrome. It has been reported that patients with rare single gene disorders or common genetic variants may develop features of the metabolic syndrome [5]. However, the metabolic syndrome rarely occurs in non-obese, non-smoking individuals with a healthy lifestyle that includes physical activity and a healthy diet that emphasizes consumption of fruits, vegetables, and whole grains and moderate alcohol intake. An energy-dense diet and sedentary lifestyle are therefore key factors underpinning development of the metabolic syndrome. According to the American Heart Association/National Heart, Lung, and Blood Institute (AHA/NHLBI) scientific statement of 2005 [6], excess body fat and visceral fat in particular are at the core of the metabolic complications observed in the metabolic syndrome. Along with insulin resistance, physical inactivity, aging, and hormonal imbalance, excess visceral adipose tissue increases the risk of developing the metabolic syndrome and related complications. According to NCEP-ATP III, management of the metabolic syndrome should focus first on abdominal obesity and physical inactivity, targeting complications of excess visceral fat thereafter. Once LDL cholesterol levels are brought under control, NCEP-ATP III recommends that the best strategy for individuals with the metabolic syndrome is a weight reduction of 7 to 10% of initial body weight within 6 to 12 months. To achieve this weight loss, a daily caloric deficit of about 500 to 1,000 kilocalories should be induced through better food choices that reduce diet energy density.
Increasing physical activity can also speed the process. Recommendations include at least 30 minutes of moderate-intensity physical activity/exercise, such as brisk walking, most days of the week. Increasing exercise duration and frequency can cause even greater weight loss and have a positive impact on cardiometabolic risk alterations found in patients with excess visceral fat. Since waist circumference is a crude marker of abdominal obesity, NCEP-ATP III suggests measuring waist circumference as a key criterion to diagnose the metabolic syndrome.
Beyond elevated LDL cholesterol, the atherogenic dyslipidemia of the metabolic syndrome has been identified as a marker of abnormal lipolytic activity of visceral adipose tissue and associated ectopic fat deposition. These markers include elevated triglyceride and apolipoprotein B levels, higher amounts of triglyceride-enriched small, dense LDL and HDL particles, and low HDL cholesterol. In the proposed criteria for diagnosing the metabolic syndrome, fasting triglycerides should be equal to or above 1.7 mmol/l (150 mg/dl) (or the patient should be on drug treatment for elevated triglycerides) and HDL cholesterol levels should be below 1.04 mmol/l (40 mg/dl) in men and below 1.29 mmol/l (50 mg/dl) in women (or the patient should be on drug treatment for low HDL cholesterol) [1]. Although the primary target is elevated LDL cholesterol levels (even in the metabolic syndrome), the secondary therapeutic target of the atherogenic dyslipidemia of the metabolic syndrome is non-HDL cholesterol (total cholesterol minus HDL cholesterol, which includes the cholesterol associated with the atherogenic lipoproteins VLDL, IDL, and LDL). To achieve non-HDL cholesterol goals, patients can benefit from intensive LDL cholesterol-lowering therapy or from adding a fibrate or nicotinic acid to their current pharmacological treatment.
Patients with triglyceride levels above 5.6 mmol/l (500 mg/dl) can also benefit from a fibrate or nicotinic acid in order to prevent pancreatitis. The tertiary target of therapy is HDL cholesterol, and guidelines recommend lifestyle therapy to raise HDL cholesterol levels.
High blood pressure is another feature of the metabolic syndrome closely associated with abdominal obesity and insulin resistance [7]. In both men and women, suggested categorical cutpoints for elevated blood pressure in the presence of the metabolic syndrome are 130 mm Hg for systolic blood pressure and 85 mm Hg for diastolic blood pressure. For slightly elevated blood pressure (≥120/80 mm Hg) (or drug treatment for elevated blood pressure or history of hypertension), patients are encouraged to initiate or maintain lifestyle therapy, paying special attention to sodium intake. Patients with a higher blood pressure (≥140/90 mm Hg) should aim to reduce it by adding blood pressure medication, such as angiotensin I converting enzyme (ACE)-inhibitors, to lifestyle therapy.
Impaired fasting glucose (IFG), a powerful predictor of type 2 diabetes, is also often seen in patients with the metabolic syndrome [8]. NCEP-ATP III criteria for IFG were revised in 2005 to meet American Diabetes Association (ADA) recommendations [9]. The cutoff value was therefore lowered from 6.1 mmol/l (110 mg/dl) to 5.6 mmol/l (100 mg/dl) for both men and women (or drug treatment for elevated fasting glucose). Several studies have documented the benefits of physical activity in patients with IFG [10,11]. NCEP-ATP III guidelines stress weight reduction and increased physical activity to delay the metabolic syndrome’s progression to type 2 diabetes, as predicted by elevated fasting glucose concentrations.
Although NCEP-ATP III did not include markers of the pro-inflammatory state among its five clinical criteria, it strongly encouraged adopting lifestyle therapies to lessen the chronic inflammation associated with the metabolic syndrome. This inflammation is characterized by high levels of interleukin-6, tumour necrosis factor-α, and C-reactive protein. Although this issue remains a matter of debate, CRP is thought to increase the risk of cardiovascular disease (CVD) and has been proposed to be added to other cardiovascular risk factors to optimize global CVD risk prediction [12].
A pro-thrombotic state is another feature of the metabolic syndrome linked to visceral obesity, insulin resistance, and atherogenic dyslipidemia. Adipose tissue-derived free fatty acids are known to exacerbate hepatic synthesis and excretion of clotting factors [13]. Hypersecretion of triglyceride-rich lipoproteins by the liver also increases concentrations of the plasminogen activator inhibitor-1 (PAI-1). Other known thrombosis markers include fibrinogen, tissue factor, and factors VII and VIII. As with the pro-inflammatory state, NCEP-ATP III clinical criteria for the metabolic syndrome do not consider markers of thrombosis. However, NCEP-ATP III recommends the use of other therapies, such as low-dose aspirin, in conjunction with lifestyle therapies to reduce the risk of thrombotic events. For more information, refer to Complications of Visceral Obesity and Managing CMR sections.
NCEP-ATP III Clinical Tools for Diagnosing the Metabolic Syndrome and Type 2 Diabetes/CVD Risk
Since the publication of NCEP-ATP III guidelines for diagnosing the metabolic syndrome, several population-based studies have examined the relationship between these criteria and the risk of developing CVD and/or type 2 diabetes. Most studies have found a positive relationship between the metabolic syndrome and CVD risk. This relationship is generally stronger when diabetes incidence is considered as an endpoint given the significant relationship between the metabolic syndrome and diabetes risk.
The Framingham Heart Offspring Study evaluated the incidence of CVD, CHD, and type 2 diabetes in individuals with the metabolic syndrome according to NCEP-ATP III clinical criteria [14]. The study sample included 3,323 men and women who were followed for eight years. Age-adjusted relative risk (RR) for men with the metabolic syndrome was 2.88 (95% CI, 1.99-4.16) for incident CVD and 6.92 (95% CI, 4.47-10.81) for onset of type 2 diabetes. Age-adjusted relative CVD risk for women with the metabolic syndrome was 2.25 (95% CI, 1.31-3.88). Type 2 diabetes incidence in women with the metabolic syndrome was similar to that of men (RR=6.90, 95% CI, 4.34-10.94). Results of the Framingham Heart Offspring Study suggest that the metabolic syndrome as identified by NCEP-ATP III clinical criteria predicts CVD and CHD risk, and that the metabolic syndrome is an even stronger predictor of type 2 diabetes.
In the Atherosclerosis Risk In Communities (ARIC) study, McNeill et al. [15] sought to determine the relationship between the metabolic syndrome and relative CHD/stroke risk among 12,089 black and white middle-aged individuals over an 11-year follow-up. In men, RR for CHD was 1.46 (95% CI, 1.23-1.74) after adjusting for age, race/ARIC centre, LDL cholesterol levels, and smoking. Women had a similar RR (RR=2.05, 95% CI, 1.59-2.64). In the ARIC study, elevated blood pressure and low HDL cholesterol were the features of the metabolic syndrome with the strongest ties to CHD risk.
The Hoorn Study is another population-based cohort study that evaluated incidence of fatal and non-fatal CVD in 1,364 men and women 50 to 75 years of age with and without metabolic syndrome over a 10-year follow-up [16]. In men, the hazard ratio for fatal and non-fatal CVD was 1.91 (95% CI, 1.31-2.79), and the hazard ratio for fatal and non-fatal CVD in women was 1.68 (95% CI, 1.11-2.55). The metabolic syndrome clinical criteria of the World Health Organization, European Group for the Study of Insulin Resistance, and American College of Endocrinology were also evaluated. Results are presented in Comparison of Screening Tools.
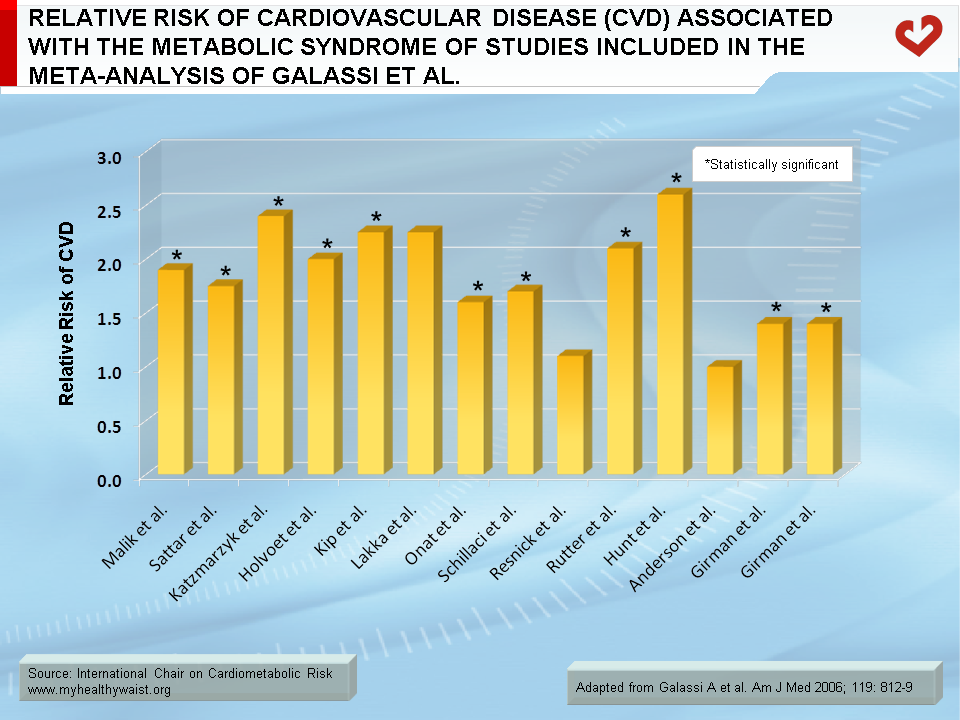
The findings of three meta-analyses that used NCEP-ATP III clinical criteria to evaluate the association between metabolic syndrome and CVD were published. Galassi et al. [17] examined a total of 21 prospective studies, 15 of which used NCEP-ATP III clinical criteria for diagnosing the metabolic syndrome. In these 15 studies, compared to individuals without the metabolic syndrome, individuals with the metabolic syndrome had a relative CVD risk of 1.61 (95% CI, 1.42-1.83). The authors also found that the metabolic syndrome was positively and significantly associated with all-cause mortality, CVD mortality, CVD incidence, CHD incidence, and stroke incidence. Subgroup analyses also suggested that the association between the metabolic syndrome and incident CVD was stronger in women than in men. The Figure provides an overview of some of the studies that were considered in the meta-analysis using NCEP-ATP III clinical criteria. Another meta-analysis of 22 studies was performed by Gami et al. [18]. This study used NCEP-ATP III clinical criteria (or modified NCEP-ATP III criteria). The RR for cardiovascular events was 1.67 when NCEP-ATP III criteria were available. In accordance with the other meta-analysis [17], this association was found to be stronger in women than in men. Interestingly, the meta-analysis by Gami et al. [18] suggested that the metabolic syndrome better predicted cardiovascular risk than the sum of its individual components. Finally, the meta-analysis by Mottillo et al. [19] identified 87 studies, which included 951,083 patients. Using clinical criteria of NCEP-ATP III (initial and revised criteria), the metabolic syndrome was associated with a significant increase in the risk of several outcomes such as CVD risk (RR: 2.35; 95% CI, 2.02-2.73), CVD mortality (RR: 2.40; 95% CI, 1.87-3.08), all-cause mortality (RR: 1.58; 95% CI, 1.39-1.78), myocardial infarction (RR: 1.99; 95% CI, 1.61-2.46), and stroke (RR: 2.27; 95% CI, 1.80-2.85).
Although the metabolic syndrome clearly increases RR of CVD/CHD, clinical diagnosis of the metabolic syndrome is not sufficient to adequately predict absolute CVD/CHD risk. To do so, focus must first be placed on well-established risk factors such as age, sex, LDL and HDL cholesterol, smoking, blood pressure, and diabetes.
A number of prospective studies, such as the Framingham Heart Offspring Study, the San Antonio Heart Study, and the Mexico City Diabetes Study, have reported that the presence of the metabolic syndrome as identified by NCEP-ATP III criteria is also closely related to type 2 diabetes risk [20,21]. In fact, most studies have found that the metabolic syndrome is better at predicting diabetes than CVD.
In summary, the NCEP-ATP III report is clearly a big step forward in global assessment of cardiovascular risk factors and related risk. By stressing physical activity and healthy nutritional habits, it aims to reduce abdominal obesity and, consequently, lower the cardiovascular risk associated with the metabolic syndrome.
For updated information, please visit the National Heart, Lung, and Blood Institute website.
References
-
Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001; 285: 2486-97.
PubMed ID: 11368702
-
Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). The Guidelines. http://www.nhlbi.nih.gov/guidelines/cholesterol/index.htm, last accessed November 2020.
PubMed ID:
-
Després JP and Lemieux I. Abdominal obesity and metabolic syndrome. Nature 2006; 444: 881-7.
PubMed ID: 17167477
-
Grundy SM. What is the contribution of obesity to the metabolic syndrome? Endocrinol Metab Clin North Am 2004; 33: 267-82
PubMed ID: 15158519
-
Pollex RL and Hegele RA. Genetic determinants of the metabolic syndrome. Nat Clin Pract Cardiovasc Med 2006; 3: 482-9.
PubMed ID: 16932765
-
Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005; 112: 2735-52.
PubMed ID: 16157765
-
Poirier P, Lemieux I, Mauriège P, et al. Impact of waist circumference on the relationship between blood pressure and insulin: the Quebec Health Survey. Hypertension 2005; 45: 363-7.
PubMed ID: 15668356
-
Unwin N, Shaw J, Zimmet P, et al. Impaired glucose tolerance and impaired fasting glycaemia: the current status on definition and intervention. Diabet Med 2002; 19: 708-23.
PubMed ID: 12207806
-
Genuth S. Lowering the criterion for impaired fasting glucose is in order. Diabetes Care 2003; 26: 3331-2.
PubMed ID: 14633824
-
Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002; 346: 393-403.
PubMed ID: 11832527
-
Tuomilehto J, Lindstrom J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001; 344: 1343-50.
PubMed ID: 11333990
-
Ridker PM. High-sensitivity C-reactive protein, inflammation, and cardiovascular risk: from concept to clinical practice to clinical benefit. Am Heart J 2004; 148: S19-26.
PubMed ID: 15211329
-
Juhan-Vague I, Morange PE and Alessi MC. The insulin resistance syndrome: implications for thrombosis and cardiovascular disease. Pathophysiol Haemost Thromb 2002; 32: 269-73.
PubMed ID: 13679655
-
Wilson PW, D’Agostino RB, Parise H, et al. Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation 2005; 112: 3066-72.
PubMed ID: 16275870
-
McNeill AM, Rosamond WD, Girman CJ, et al. The metabolic syndrome and 11-year risk of incident cardiovascular disease in the Atherosclerosis Risk in Communities study. Diabetes Care 2005; 28: 385-90.
PubMed ID: 15677797
-
Dekker JM, Girman C, Rhodes T, et al. Metabolic syndrome and 10-year cardiovascular disease risk in the Hoorn Study. Circulation 2005; 112: 666-73.
PubMed ID: 16061755
-
Galassi A, Reynolds K and He J. Metabolic syndrome and risk of cardiovascular disease: a meta-analysis. Am J Med 2006; 119: 812-9.
PubMed ID: 17000207
-
Gami AS, Witt BJ, Howard DE, et al. Metabolic syndrome and risk of incident cardiovascular events and death: a systematic review and meta-analysis of longitudinal studies. J Am Coll Cardiol 2007; 49: 403-14.
PubMed ID: 17258085
-
Mottillo S, Filion KB, Genest J, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol 2010; 56: 1113-32.
PubMed ID: 20863953
-
Rutter MK, Meigs JB, Sullivan LM, et al. Insulin resistance, the metabolic syndrome, and incident cardiovascular events in the Framingham Offspring Study. Diabetes 2005; 54: 3252-7.
PubMed ID: 16249452
-
Stern MP, Williams K, Gonzalez-Villalpando C, et al. Does the metabolic syndrome improve identification of individuals at risk of type 2 diabetes and/or cardiovascular disease? Diabetes Care 2004; 27: 2676-81.
PubMed ID: 15505004
 CLOSE
CLOSE
Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001; 285: 2486-97.
PubMed ID: 11368702 CLOSE
CLOSE
Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). The Guidelines. http://www.nhlbi.nih.gov/guidelines/cholesterol/index.htm, last accessed November 2020.
PubMed ID: CLOSE
CLOSE
Després JP and Lemieux I. Abdominal obesity and metabolic syndrome. Nature 2006; 444: 881-7.
PubMed ID: 17167477 CLOSE
CLOSE
Grundy SM. What is the contribution of obesity to the metabolic syndrome? Endocrinol Metab Clin North Am 2004; 33: 267-82
PubMed ID: 15158519 CLOSE
CLOSE
Pollex RL and Hegele RA. Genetic determinants of the metabolic syndrome. Nat Clin Pract Cardiovasc Med 2006; 3: 482-9.
PubMed ID: 16932765 CLOSE
CLOSE
Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005; 112: 2735-52.
PubMed ID: 16157765 CLOSE
CLOSE
Poirier P, Lemieux I, Mauriège P, et al. Impact of waist circumference on the relationship between blood pressure and insulin: the Quebec Health Survey. Hypertension 2005; 45: 363-7.
PubMed ID: 15668356 CLOSE
CLOSE
Unwin N, Shaw J, Zimmet P, et al. Impaired glucose tolerance and impaired fasting glycaemia: the current status on definition and intervention. Diabet Med 2002; 19: 708-23.
PubMed ID: 12207806 CLOSE
CLOSE
Genuth S. Lowering the criterion for impaired fasting glucose is in order. Diabetes Care 2003; 26: 3331-2.
PubMed ID: 14633824 CLOSE
CLOSE
Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002; 346: 393-403.
PubMed ID: 11832527 CLOSE
CLOSE
Tuomilehto J, Lindstrom J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001; 344: 1343-50.
PubMed ID: 11333990 CLOSE
CLOSE
Ridker PM. High-sensitivity C-reactive protein, inflammation, and cardiovascular risk: from concept to clinical practice to clinical benefit. Am Heart J 2004; 148: S19-26.
PubMed ID: 15211329 CLOSE
CLOSE
Juhan-Vague I, Morange PE and Alessi MC. The insulin resistance syndrome: implications for thrombosis and cardiovascular disease. Pathophysiol Haemost Thromb 2002; 32: 269-73.
PubMed ID: 13679655 CLOSE
CLOSE
Wilson PW, D’Agostino RB, Parise H, et al. Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation 2005; 112: 3066-72.
PubMed ID: 16275870 CLOSE
CLOSE
McNeill AM, Rosamond WD, Girman CJ, et al. The metabolic syndrome and 11-year risk of incident cardiovascular disease in the Atherosclerosis Risk in Communities study. Diabetes Care 2005; 28: 385-90.
PubMed ID: 15677797 CLOSE
CLOSE
Dekker JM, Girman C, Rhodes T, et al. Metabolic syndrome and 10-year cardiovascular disease risk in the Hoorn Study. Circulation 2005; 112: 666-73.
PubMed ID: 16061755 CLOSE
CLOSE
Galassi A, Reynolds K and He J. Metabolic syndrome and risk of cardiovascular disease: a meta-analysis. Am J Med 2006; 119: 812-9.
PubMed ID: 17000207 CLOSE
CLOSE
Gami AS, Witt BJ, Howard DE, et al. Metabolic syndrome and risk of incident cardiovascular events and death: a systematic review and meta-analysis of longitudinal studies. J Am Coll Cardiol 2007; 49: 403-14.
PubMed ID: 17258085 CLOSE
CLOSE
Mottillo S, Filion KB, Genest J, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol 2010; 56: 1113-32.
PubMed ID: 20863953 CLOSE
CLOSE
Rutter MK, Meigs JB, Sullivan LM, et al. Insulin resistance, the metabolic syndrome, and incident cardiovascular events in the Framingham Offspring Study. Diabetes 2005; 54: 3252-7.
PubMed ID: 16249452 CLOSE
CLOSE
Stern MP, Williams K, Gonzalez-Villalpando C, et al. Does the metabolic syndrome improve identification of individuals at risk of type 2 diabetes and/or cardiovascular disease? Diabetes Care 2004; 27: 2676-81.
PubMed ID: 15505004