Usefulness of Hypertriglyceridemic Waist
Evaluating CMR - Metabolic Syndrome and Type 2 Diabetes/CVD RiskKey Points
- Hypertriglyceridemic waist (elevated waist girth and triglyceride concentrations) could be a simple and inexpensive way to identify individuals with high levels of visceral fat and the features of the metabolic syndrome.
- The simultaneous presence of an elevated waist circumference and high triglyceride levels increases relative risk of CHD.
- Hypertriglyceridemic waist increases the risk of type 2 diabetes.
- A diagnosis of hypertriglyceridemic waist is not sufficient, however, to assess global CHD risk.
History of Hypertriglyceridemic Waist
There is growing evidence that variables other than traditional risk factors may facilitate the identification of individuals at elevated risk of coronary heart disease (CHD). In this regard, prospective data from the Québec Cardiovascular Study showed that some features of the metabolic syndrome (the atherogenic metabolic triad: elevated insulin and apolipoprotein B concentrations and small LDL particles) often found in abdominally obese individuals substantially increase CHD risk, while individuals without this triad of unconventional risk markers of abdominal obesity and the metabolic syndrome have a lower CHD risk [1]. Furthermore, the risk associated with these features remained highly significant even after traditional risk factors such as LDL cholesterol, HDL cholesterol, and triglyceride levels were taken into account [1]. These findings suggest that paying attention to markers of the metabolic syndrome in abdominally obese patients could refine CHD risk assessment beyond the risk factors traditionally used in clinical practice. Since several markers of the metabolic syndrome cannot be used on a large scale in clinical practice due to accessibility, cost, and standardization problems (with the exception of apolipoprotein B, which is now standardized [2]), a research group from Université Laval sought to develop a simple and inexpensive screening tool to help general practitioners identify individuals at risk of developing CHD because of the presence of abdominal obesity and features of the metabolic syndrome.
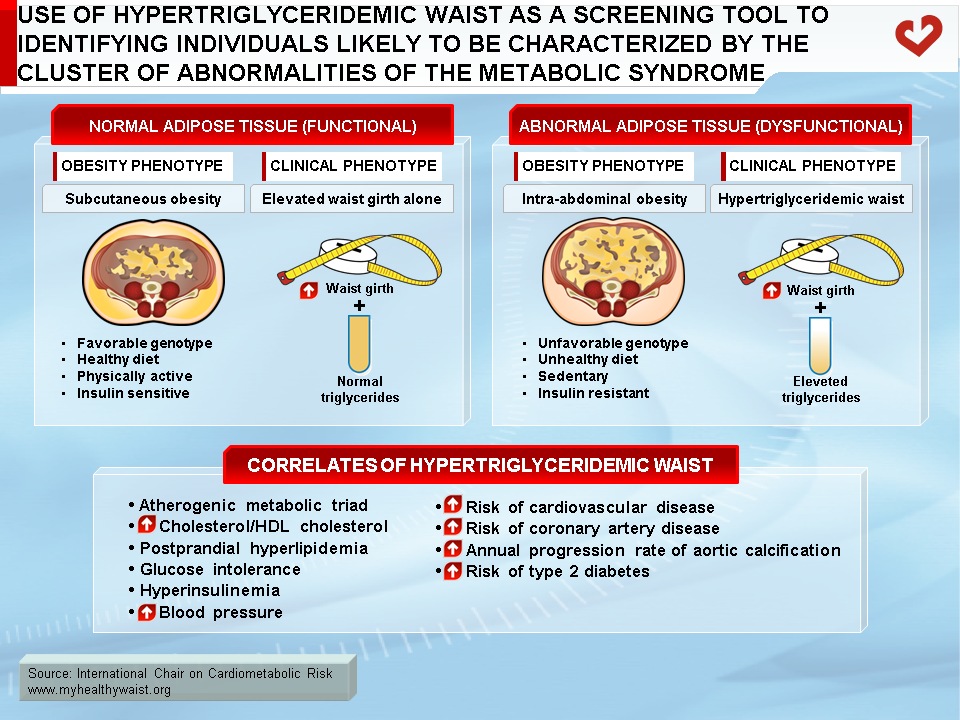
The simultaneous presence of an increased waist circumference and elevated fasting triglyceride concentrations (hypertriglyceridemic waist) could be used as an initial screening phenotype to identify a subgroup of patients likely to be characterized by features of the metabolic syndrome, such as fasting hyperinsulinemia, elevated apolipoprotein B, and higher amounts of small LDL particles: the atherogenic metabolic triad (Figure) [3]. It is important to emphasize that waist girth should be measured and interpreted along with fasting triglyceride concentrations because not all individuals with an elevated waist girth have visceral fat and are at high risk of type 2 diabetes or cardiovascular disease (CVD).
It was previously reported that in the presence of an elevated waist circumference, fasting hypertriglyceridemia could be a marker of the patient’s relative inability to manage and store extra energy in the subcutaneous fat depot, which should have acted as a protective “metabolic sink” under this model [4], allowing the rapid clearance and storage of excess dietary triglycerides in subcutaneous adipose tissue. Abdominal obesity can therefore have two faces: 1) abdominal obesity in isolation (often associated with excess subcutaneous fat) or 2) abdominal obesity associated with metabolic complications (often found in patients with excess visceral adiposity) (Figure). As the latter condition increases type 2 diabetes and CHD risk, there was a need to develop a simple algorithm to identify individuals with the metabolic syndrome. Hyperinsulinemia and elevated apolipoprotein B concentrations were found to be closely linked to visceral adipose tissue accumulation [5]. Visceral adipose tissue can be directly and precisely measured using imaging techniques such as computed tomography and magnetic resonance imaging, but these methods are expensive and computed tomography involves radiation exposure. However, it was shown that measuring waist circumference could serve as a crude surrogate marker of visceral adipose tissue accumulation as well as insulinemia and apolipoprotein B levels [6-8]. On the other hand, fasting triglyceride levels have been linked to the presence of small, dense LDL [9].
Based on the ties between waist girth, triglyceride concentrations, and features of the metabolic syndrome, sensitivity and specificity analyses were performed in a sample of Caucasian men 28 to 63 years of age. They revealed that the best cutoffs for determining the presence/absence of features of the atherogenic metabolic triad were 90 cm for waist circumference and 2.0 mmol/l for fasting triglyceride concentrations [3]. These simple clinical criteria were validated and reported before the publication of the National Cholesterol Education Program-Adult Treatment Panel III (NCEP-ATP III) guidelines. In the initial study, only 10% of men with a low waist girth (<90 cm and triglyceride concentrations <2.0 mmol/l) had the atherogenic metabolic triad of abdominal obesity. However, 84% of men with hypertriglyceridemic waist (waist girth ≥90 cm and triglycerides ≥2.0 mmol/l) had the atherogenic metabolic triad. In women, sensitivity and specificity analyses have allowed to determine cutoff values of 85 cm for waist circumference and of 2.0 mmol/l for fasting triglyceride concentrations [10].
Since the publication of the first paper describing the hypertriglyceridemic waist concept [3], several studies worldwide have examined how this simple screening phenotype can help identify individuals likely to have features of the metabolic syndrome or report associations with type 2 diabetes and CHD [3,10-26]. Morever, results of two meta-analyses revealed that the hypertriglyceridemic waist phenotype was associated with an abnormal glucose metabolism and an increased risk of type 2 diabetes [27-28]. Although slightly different cutoff values for waist circumference and triglyceride levels have been used across studies, the conclusions reached have been similar.
Prevalence of Hypertriglyceridemic Waist
Prevalence data from a representative sample of adults of the province of Québec aged 18 to 74 (Québec Health Survey) has enabled the number of men with hypertriglyceridemic waist in Québec to be quantified [10]. Study results indicated that 19% of adult men in the Québec Health Survey had an elevated waist circumference (≥90 cm) and hypertriglyceridemia (≥2.0 mmol/l) [11]. This percentage increased to 29.2% in the subgroup of men aged 40 to 65. Though different cutoffs were used, the prevalence of this phenotype was similar (19%) in the Tehran Lipid and Glucose Study, which involved more than 4,000 men [14]. The prevalence of hypertriglyceridemic waist was also quantified in a sample of 4,448 men and 4,735 women from the third National Health and Nutrition Examination Survey (NHANES III) [19]. In this study, Kahn and Valdez [19] found that, irrespective of sex, the estimated prevalence of the simultaneous presence of an elevated waist circumference and increased triglyceride levels was about 25%. They also found that the estimated prevalence of this phenotype increased with age and was higher (>40%) in men and women aged 55 to 74. A publication from the “SUpplémentation en VItamines et Minéraux Anti-oXydants” (SU.VI.MAX) study also revealed that 12.1% of their sample of middle-aged men had hypertriglyceridemic waist [17]. Finally, the prevalence of hypertriglyceridemic waist has been quantified in a meta-analysis involving more than 90,000 individuals [28]. The prevalence reached 18% in men and 19% in women [28]. Since obesity, especially abdominal obesity, is fast increasing [29], the prevalence of hypertriglyceridemic waist is expected to follow suit. With overweight/obesity in countries such as Canada, Australia, and the United States already afflicting 50% of the population, hypertriglyceridemic waist would allow physicians to focus on the subgroup of overweight/obese patients (with hypertriglyceridemic waist) at greatest risk of type 2 diabetes and CHD, rather than treating half their patients as a blanket measure.
Hypertriglyceridemic Waist and Coronary Risk
Additional findings from the first publication on hypertriglyceridemic waist revealed that only the simultaneous presence of elevated waist girth and triglyceride concentrations was associated with coronary artery disease (CAD) assessed by angiography [3]. In a sample of 287 men who underwent an angiographic procedure for symptoms of CAD, men whose waist circumference and triglyceride levels were elevated had higher odds of being diagnosed with significant CAD than men with a waist circumference <90 cm and triglyceride concentrations <2.0 mmol/l (odds ratio: 3.6, 95% CI: 1.17-10.93, p<0.03). In isolation, an elevated waist circumference or hypertriglyceridemia did not significantly increase CAD. Furthermore, in a small study of heart transplant patients, the odds of CAD increased fourfold, though this finding was not statistically significant because of the small sample size (n=83) [13]. The usefulness of hypertriglyceridemic waist and the NCEP-ATP III clinical criteria in establishing risk of all-cause and cardiovascular mortality as well as predicting the annual progression rate of aortic calcification was examined in a sample of more than 550 women followed for 8.5 years [18]. Survival curves analysis for all-cause or cardiovascular mortality indicated that survival rates dropped significantly in women with an elevated waist girth and high triglyceride concentrations compared to women without these conditions. Moreover, relative risk for all-cause mortality (hazard ratio: 2.2, 95% CI: 1.3-3.6, p<0.01) and cardiovascular death (hazard ratio: 4.7, 95% CI: 2.2-9.8, p<0.001) associated with hypertriglyceridemic waist was significant even after adjusting for age, smoking, and LDL cholesterol. These findings were repeated in a sub-analysis that excluded women with diabetes. The annual progression rate of aortic calcification was significantly greater in women meeting the NCEP-ATP III criteria or with hypertriglyceridemic waist. However, the highest rates were observed in subgroups with both high waist girth and triglyceride levels, regardless of the presence/absence of NCEP-ATP III criteria. These criteria alone were not as effective as hypertriglyceridemic waist in predicting the annual progression rate of aortic calcification.
In a 7.5-year prospective study (the SU.VI.MAX study) of 3,430 middle-aged men, using subjects with low waist girth and low triglyceride concentrations as the reference group, investigators reported that the risk of developing CVD over the follow-up only increased significantly among men with hypertriglyceridemic waist after adjusting for age, active smoking, physical activity, systolic blood pressure, diastolic blood pressure, and fasting blood glucose (relative risk: 2.13, 95% CI: 1.21-3.76) [17]. These results were confirmed in the large EPIC-Norfolk prospective study where men and women who had both an increased waist circumference and hypertriglyceridemia had the lowest probability of remaining CAD-free (p<0.001 for both sexes) [30].
Although it has been reported that hyperglycemia (even in the nondiabetic range) increases CAD [31,32], it is not clear whether it is dysglycemia that has a direct impact on CAD risk or the metabolic syndrome frequently observed among dysglycemic patients. This question has been examined, and the results showed that the presence/absence of hypertriglyceridemic waist modulated hyperglycemia-related CAD risk in men [15]. For instance, in the absence of hypertriglyceridemic waist, men with fasting hyperglycemia (in isolation) were not at increased risk of CAD. However, the CAD risk associated with hypertriglyceridemic waist significantly increased in both men with normal glucose levels (<6.1 mmol/l) or with an impaired fasting glucose concentration (6.1-6.9 mmol/l). An investigation of a large sample of men and women from the Hoorn study confirmed these results [26].
The combination of a large waist circumference with elevated triglyceride concentrations increased CVD risk among individuals with either normal or abnormal glucose levels (hazard ratio: 1.82; 95% CI: 1.27-2.62 and 2.68; 95% CI: 1.89-3.81, respectively). Another prospective study tested the hypothesis that hypertriglyceridemic waist, as a covariate of metabolic syndrome features, predicted premature CAD among patients with glucose intolerance or type 2 diabetes [33]. The sample included 1,990 men and women, including 592 patients with impaired glucose tolerance or type 2 diabetes. Survival models revealed that among patients with impaired glucose tolerance or type 2 diabetes, those with hypertriglyceridemic waist experienced their first CAD symptoms 5 years earlier than those without this phenotype. This elevated and earlier risk of CAD was statistically significant (hazard ratio: 2.0; 95% CI: 1.2-3.7, p=0.02). Thus, although the relationship between glucose levels and CVD risk is well established, these findings suggest that the presence/absence of hypertriglyceridemic waist could be useful to clinicians in refining assessment of CVD risk due to a dysglycemic or prediabetic state. The presence of abdominal obesity and hypertriglyceridemia should therefore be a warning sign for physicians.
Hypertriglyceridemic Waist and Diabetes
Hypertriglyceridemic waist has also been shown to be associated with increased type 2 diabetes rates in adult men and women [11,19]. Using data from NHANES III, both men and women aged 40 to 74 with hypertriglyceridemic waist were found to have an estimated diabetes prevalence of 25.4%, with this prevalence being only 8.0% in subjects without this phenotype (relative risk: 3.2: 95% CI: 2.4-4.0) [19]. The odds of developing diabetes was also markedly higher in men of the Québec Health Survey with an elevated waist circumference and high triglyceride concentration [11]. A twelvefold increase in the prevalent odds ratio of diabetes (95% CI: 5.1-27.9, p<0.0001) was observed in men with hypertriglyceridemic waist compared to the reference group of men with both low waist girth and triglyceride levels. The prevalent odds ratio was not as high among obese (body mass index (BMI) ≥30 kg/m2) versus normal weight men (odds ratio: 7; 95% CI: 3.4-13.9, p<0.0001). Furthermore, the metabolic profile of men with hypertriglyceridemic waist was as worse as, if not worse than, that of men with diabetes [11]. The usefulness of hypertriglyceridemic waist to identify individuals with type 2 diabetes has been documented in two meta-analyses [27-28]. The odds ratio for diabetes was 2.69 (95% CI: 2.40-3.01) in a meta-analysis involving more than 190,000 individuals [27] and 4.18 (95% CI: 3.55-4.92) in another meta-analysis involving more than 34,000 individuals [28].
Hypertriglyceridemic Waist Predicts Metabolic Abnormalities
Hypertriglyceridemic waist can also be useful in clinical practice to detect individuals likely to have features of the metabolic syndrome, such as an elevated cholesterol/HDL cholesterol ratio, postprandial hyperlipidemia, hyperinsulinemia, and a dyslipidemic profile typically found in subjects with abdominal obesity. In this regard, Solati et al. [14] reported that 75% of men of the Tehran Lipid and Glucose Study with hypertriglyceridemic waist had four to six risk factors (cholesterol, LDL cholesterol, HDL cholesterol, systolic blood pressure, diastolic blood pressure, and BMI). Other studies have also validated the ability of hypertriglyceridemic waist to identify individuals at high risk of CVD [12,16,19-22]. LaMonte et al. [12] have published evidence that more than two-thirds of women with elevated waist girth and triglyceride concentrations also had hyperinsulinemia as well as increased apolipoprotein B and LDL cholesterol levels. Furthermore, a clear relationship between hypertriglyceridemic waist and the cholesterol/HDL cholesterol ratio, a well-known strong predictor of CHD [34,35], has been reported in several study populations [11,15,19,22]. The prevalence of subjects with a cholesterol/HDL cholesterol ratio ≥6 was almost 50%, whereas it was only 3% among men with both low waist girth and normal triglyceride concentrations (10). Carriers of the hypertriglyceridemic waist phenotype also have deteriorated plasma glucose-insulin homeostasis compared to individuals without this phenotype [11,12,19,21,22]. In addition, a postprandial study revealed that men with hypertriglyceridemic waist had the greatest increase in triglyceride concentrations during the postprandial state compared to control subjects [16]. The latter study also indicated that this phenotype was better at identifying a hyperlipidemic state during the postprandial phase than elevated waist circumference or hypertriglyceridemia measured in isolation.
Hypertriglyceridemic Waist and Global CHD Risk
Although hypertriglyceridemic waist is very helpful in clinical practice as a screening tool for identifying patients with the metabolic syndrome, the presence of hypertriglyceridemic waist does not necessarily mean that the patient is at high absolute risk of CHD. The diagnosis of hypertriglyceridemic waist should therefore not be considered in isolation to quantify global CHD risk. Rather, improved global risk assessment algorithms are needed to quantify diabetes and CVD risk resulting from the presence of classical risk factors as well as capture the additional risk caused by abdominal obesity/insulin resistance-related metabolic markers (metabolic syndrome). This overall risk is referred to as global “cardiometabolic risk” [4]. Cardiometabolic risk encompasses the global risk of CVD and type 2 diabetes associated with classical risk factors, while also taking into account the additional contribution of abdominal obesity/insulin resistance and related metabolic markers (to be identified) to global CVD risk. Whether the clinical criteria of the metabolic syndrome add to global CVD risk remains uncertain and is a matter of debate. Only additional prospective studies to directly measure sophisticated metabolic markers and visceral and subcutaneous adiposity can answer this important question. Once these findings are released, we should be better able to define what constitutes a high-risk abdominal obesity phenotype in various regions of the world and elucidate key determinants of risk in different populations.
In summary, because the metabolic syndrome increases the risk of type 2 diabetes and CVD, a number of organizations have proposed screening approaches to identify patients with features of the metabolic syndrome. However, the range of variables and cutoffs proposed has sometimes left clinicians feeling confused and perplexed. Based on evidence that waist circumference and triglycerides may be as good as other, more demanding approaches such as the NCEP-ATP III criteria, hypertriglyceridemic waist may be the simplest tool available for quick initial screening of the metabolic syndrome in clinical practice. However, additional prospective studies are necessary to validate fasting triglyceride concentrations and waist circumference cutoff values in various ethnic populations, in both sexes, and across different age groups.
References
-
Lamarche B, Tchernof A, Mauriège P, et al. Fasting insulin and apolipoprotein B levels and low-density lipoprotein particle size as risk factors for ischemic heart disease. JAMA 1998; 279: 1955-61.
PubMed ID: 9643858
-
Marcovina S and Packard CJ. Measurement and meaning of apolipoprotein AI and apolipoprotein B plasma levels. J Intern Med 2006; 259: 437-46.
PubMed ID: 16629849
-
Lemieux I, Pascot A, Couillard C, et al. Hypertriglyceridemic waist. A marker of the atherogenic metabolic triad (hyperinsulinemia, hyperapolipoprotein B, small, dense LDL) in men? Circulation 2000; 102: 179-84.
PubMed ID: 10889128
-
Després JP and Lemieux I. Abdominal obesity and metabolic syndrome. Nature 2006; 444: 881-7.
PubMed ID: 17167477
-
Lemieux S, Prud’homme D, Tremblay A, et al. Anthropometric correlates of changes in visceral adipose tissue over 7 years in women. Int J Obes Relat Metab Disord 1996; 20: 618-24.
PubMed ID: 8817355
-
Lemieux S, Prud’homme D, Bouchard C, et al. A single threshold value of waist girth identifies normal-weight and overweight subjects with excess visceral adipose tissue. Am J Clin Nutr 1996; 64: 685-93.
PubMed ID: 8901786
-
Ross R, Fortier L and Hudson R. Separate associations between visceral and subcutaneous adipose tissue distribution, insulin and glucose levels in obese women. Diabetes Care 1996; 19: 1404-11.
PubMed ID: 8941472
-
Okosun IS, Prewitt TE, Liao Y, et al. Association of waist circumference with ApoB to ApoAI ratio in black and white Americans. Int J Obes Relat Metab Disord 1999; 23: 498-504.
PubMed ID: 10375053
-
McNamara JR, Jenner JL, Li Z, et al. Change in LDL particle size is associated with change in plasma triglyceride concentration. Arterioscler Thromb 1992; 12: 1284-90.
PubMed ID: 1420088
-
Blackburn P, Lemieux I, Lamarche B, et al. Type 2 diabetes without the atherogenic metabolic triad does not predict angiographically assessed coronary artery disease in women. Diabetes Care 2008; 31: 170-172.
PubMed ID: 17934152
-
Lemieux I, Alméras N, Mauriège P, et al. Prevalence of “hypertriglyceridemic waist” in men who participated in the Quebec Health Survey: association with atherogenic and diabetogenic metabolic risk factors. Can J Cardiol 2002; 18: 725-32.
PubMed ID: 12167959
-
LaMonte MJ, Ainsworth BE, DuBose KD, et al. The hypertriglyceridemic waist phenotype among women. Atherosclerosis 2003; 171: 123-30.
PubMed ID: 14642414
-
Sénéchal M, Lemieux I, Beucler I, et al. Features of the metabolic syndrome of “hypertriglyceridemic waist” and transplant coronary artery disease. J Heart Lung Transplant 2005; 24: 819-26.
PubMed ID: 15982608
-
Solati M, Ghanbarian A, Rahmani M, et al. Cardiovascular risk factors in males with hypertriglycemic waist (Tehran Lipid and Glucose Study). Int J Obes Relat Metab Disord 2004; 28: 706-9.
PubMed ID: 14770189
-
St-Pierre J, Lemieux I, Vohl MC, et al. Contribution of abdominal obesity and hypertriglyceridemia to impaired fasting glucose and coronary artery disease. Am J Cardiol 2002; 90: 15-8.
PubMed ID: 12088772
-
Blackburn P, Lamarche B, Couillard C, et al. Postprandial hyperlipidemia: another correlate of the “hypertriglyceridemic waist” phenotype in men. Atherosclerosis 2003; 171: 327-36.
PubMed ID: 14644404
-
Czernichow S, Bruckert E, Bertrais S, et al. Hypertriglyceridemic waist and 7.5-year prospective risk of cardiovascular disease in asymptomatic middle-aged men. Int J Obes (Lond) 2007; 31: 791-6.
PubMed ID: 17047639
-
Tanko LB, Bagger YZ, Qin G, et al. Enlarged waist combined with elevated triglycerides is a strong predictor of accelerated atherogenesis and related cardiovascular mortality in postmenopausal women. Circulation 2005; 111: 1883-90.
PubMed ID: 15837940
-
Kahn HS and Valdez R. Metabolic risks identified by the combination of enlarged waist and elevated triacylglycerol concentration. Am J Clin Nutr 2003; 78: 928-34.
PubMed ID: 14594778
-
Bell D, McAuley KA, Mann J, et al. The hypertriglyceridaemic waist in New Zealand Maori. Asia Pac J Clin Nutr 2004; 13: 74-7.
PubMed ID: 15003918
-
Gazi IF, Filippatos TD, Tsimihodimos V, et al. The hypertriglyceridemic waist phenotype is a predictor of elevated levels of small, dense LDL cholesterol. Lipids 2006; 41: 647-54.
PubMed ID: 17069348
-
Hiura Y, Acklin F, Newman J, et al. Hypertriglyceridemic waist as a screening tool for CVD risk in indigenous Australian women. Ethn Dis 2003; 13: 80-4.
PubMed ID: 12723028
-
Esmaillzadeh A, Mirmiran P and Azizi F. Clustering of metabolic abnormalities in adolescents with the hypertriglyceridemic waist phenotype. Am J Clin Nutr 2006; 83: 36-46; quiz 183-4.
PubMed ID: 16400047
-
Esmaillzadeh A, Mirmiran P, Azadbakht L, et al. Prevalence of the hypertriglyceridemic waist phenotype in Iranian adolescents. Am J Prev Med 2006; 30: 52-8.
PubMed ID: 16414424
-
Esmaillzadeh A, Mirmiran P and Azizi F. Whole-grain intake and the prevalence of hypertriglyceridemic waist phenotype in Tehranian adults. Am J Clin Nutr 2005; 81: 55-63.
PubMed ID: 15640460
-
Bos G, Dekker JM and Heine RJ. Non-HDL cholesterol contributes to the “hypertriglyceridemic waist” as a cardiovascular risk factor: the Hoorn Study. Diabetes Care 2004; 27: 283-284.
PubMed ID: 14694012
-
Ma CM, Liu XL, Lu N, et al. Hypertriglyceridemic waist phenotype and abnormal glucose metabolism: a system review and meta-analysis. Endocrine 2019; 64: 469-485.
PubMed ID: 31065910
-
Ren Y, Lu X, Wang C, et al. Prevalence of hypertriglyceridemic waist and association with risk of type 2 diabetes mellitus: a meta-analysis. Diabetes Metab Res Rev 2016; 32: 405-412.
PubMed ID: 26417844
-
Ford ES, Mokdad AH and Giles WH. Trends in waist circumference among U.S. adults. Obes Res 2003; 11: 1223-31.
PubMed ID: 14569048
-
Arsenault BJ, Lemieux I, Després JP, et al. The hypertriglyceridemic-waist phenotype and the risk of coronary artery disease: results from the EPIC-Norfolk prospective population study. CMAJ 2010; 182: 1427-1432.
PubMed ID: 20643837
-
Gerstein HC and Yusuf S. Dysglycaemia and risk of cardiovascular disease. Lancet 1996; 347: 949-50.
PubMed ID: 8598762
-
Coutinho M, Gerstein HC, Wang Y, et al. The relationship between glucose and incident cardiovascular events. A metaregression analysis of published data from 20 studies of 95,783 individuals followed for 12.4 years. Diabetes Care 1999; 22: 233-40.
PubMed ID: 10333939
-
St-Pierre J, Lemieux I, Perron P, et al. Relation of the “hypertriglyceridemic waist” phenotype to earlier manifestations of coronary artery disease in patients with glucose intolerance and type 2 diabetes mellitus. Am J Cardiol 2007; 99: 369-73.
PubMed ID: 17261400
-
Kinosian B, Glick H and Garland G. Cholesterol and coronary heart disease: predicting risks by levels and ratios. Ann Intern Med 1994; 121: 641-7.
PubMed ID: 7944071
-
Lemieux I, Lamarche B, Couillard C, et al. Total cholesterol/HDL cholesterol ratio vs LDL cholesterol/HDL cholesterol ratio as indices of ischemic heart disease risk in men. The Quebec Cardiovascular Study. Arch Intern Med 2001; 161: 2685-92.
PubMed ID: 11732933
 CLOSE
CLOSE
Lamarche B, Tchernof A, Mauriège P, et al. Fasting insulin and apolipoprotein B levels and low-density lipoprotein particle size as risk factors for ischemic heart disease. JAMA 1998; 279: 1955-61.
PubMed ID: 9643858 CLOSE
CLOSE
Marcovina S and Packard CJ. Measurement and meaning of apolipoprotein AI and apolipoprotein B plasma levels. J Intern Med 2006; 259: 437-46.
PubMed ID: 16629849 CLOSE
CLOSE
Lemieux I, Pascot A, Couillard C, et al. Hypertriglyceridemic waist. A marker of the atherogenic metabolic triad (hyperinsulinemia, hyperapolipoprotein B, small, dense LDL) in men? Circulation 2000; 102: 179-84.
PubMed ID: 10889128 CLOSE
CLOSE
Després JP and Lemieux I. Abdominal obesity and metabolic syndrome. Nature 2006; 444: 881-7.
PubMed ID: 17167477 CLOSE
CLOSE
Lemieux S, Prud’homme D, Tremblay A, et al. Anthropometric correlates of changes in visceral adipose tissue over 7 years in women. Int J Obes Relat Metab Disord 1996; 20: 618-24.
PubMed ID: 8817355 CLOSE
CLOSE
Lemieux S, Prud’homme D, Bouchard C, et al. A single threshold value of waist girth identifies normal-weight and overweight subjects with excess visceral adipose tissue. Am J Clin Nutr 1996; 64: 685-93.
PubMed ID: 8901786 CLOSE
CLOSE
Ross R, Fortier L and Hudson R. Separate associations between visceral and subcutaneous adipose tissue distribution, insulin and glucose levels in obese women. Diabetes Care 1996; 19: 1404-11.
PubMed ID: 8941472 CLOSE
CLOSE
Okosun IS, Prewitt TE, Liao Y, et al. Association of waist circumference with ApoB to ApoAI ratio in black and white Americans. Int J Obes Relat Metab Disord 1999; 23: 498-504.
PubMed ID: 10375053 CLOSE
CLOSE
McNamara JR, Jenner JL, Li Z, et al. Change in LDL particle size is associated with change in plasma triglyceride concentration. Arterioscler Thromb 1992; 12: 1284-90.
PubMed ID: 1420088 CLOSE
CLOSE
Blackburn P, Lemieux I, Lamarche B, et al. Type 2 diabetes without the atherogenic metabolic triad does not predict angiographically assessed coronary artery disease in women. Diabetes Care 2008; 31: 170-172.
PubMed ID: 17934152 CLOSE
CLOSE
Lemieux I, Alméras N, Mauriège P, et al. Prevalence of “hypertriglyceridemic waist” in men who participated in the Quebec Health Survey: association with atherogenic and diabetogenic metabolic risk factors. Can J Cardiol 2002; 18: 725-32.
PubMed ID: 12167959 CLOSE
CLOSE
LaMonte MJ, Ainsworth BE, DuBose KD, et al. The hypertriglyceridemic waist phenotype among women. Atherosclerosis 2003; 171: 123-30.
PubMed ID: 14642414 CLOSE
CLOSE
Sénéchal M, Lemieux I, Beucler I, et al. Features of the metabolic syndrome of “hypertriglyceridemic waist” and transplant coronary artery disease. J Heart Lung Transplant 2005; 24: 819-26.
PubMed ID: 15982608 CLOSE
CLOSE
Solati M, Ghanbarian A, Rahmani M, et al. Cardiovascular risk factors in males with hypertriglycemic waist (Tehran Lipid and Glucose Study). Int J Obes Relat Metab Disord 2004; 28: 706-9.
PubMed ID: 14770189 CLOSE
CLOSE
St-Pierre J, Lemieux I, Vohl MC, et al. Contribution of abdominal obesity and hypertriglyceridemia to impaired fasting glucose and coronary artery disease. Am J Cardiol 2002; 90: 15-8.
PubMed ID: 12088772 CLOSE
CLOSE
Blackburn P, Lamarche B, Couillard C, et al. Postprandial hyperlipidemia: another correlate of the “hypertriglyceridemic waist” phenotype in men. Atherosclerosis 2003; 171: 327-36.
PubMed ID: 14644404 CLOSE
CLOSE
Czernichow S, Bruckert E, Bertrais S, et al. Hypertriglyceridemic waist and 7.5-year prospective risk of cardiovascular disease in asymptomatic middle-aged men. Int J Obes (Lond) 2007; 31: 791-6.
PubMed ID: 17047639 CLOSE
CLOSE
Tanko LB, Bagger YZ, Qin G, et al. Enlarged waist combined with elevated triglycerides is a strong predictor of accelerated atherogenesis and related cardiovascular mortality in postmenopausal women. Circulation 2005; 111: 1883-90.
PubMed ID: 15837940 CLOSE
CLOSE
Kahn HS and Valdez R. Metabolic risks identified by the combination of enlarged waist and elevated triacylglycerol concentration. Am J Clin Nutr 2003; 78: 928-34.
PubMed ID: 14594778 CLOSE
CLOSE
Bell D, McAuley KA, Mann J, et al. The hypertriglyceridaemic waist in New Zealand Maori. Asia Pac J Clin Nutr 2004; 13: 74-7.
PubMed ID: 15003918 CLOSE
CLOSE
Gazi IF, Filippatos TD, Tsimihodimos V, et al. The hypertriglyceridemic waist phenotype is a predictor of elevated levels of small, dense LDL cholesterol. Lipids 2006; 41: 647-54.
PubMed ID: 17069348 CLOSE
CLOSE
Hiura Y, Acklin F, Newman J, et al. Hypertriglyceridemic waist as a screening tool for CVD risk in indigenous Australian women. Ethn Dis 2003; 13: 80-4.
PubMed ID: 12723028 CLOSE
CLOSE
Esmaillzadeh A, Mirmiran P and Azizi F. Clustering of metabolic abnormalities in adolescents with the hypertriglyceridemic waist phenotype. Am J Clin Nutr 2006; 83: 36-46; quiz 183-4.
PubMed ID: 16400047 CLOSE
CLOSE
Esmaillzadeh A, Mirmiran P, Azadbakht L, et al. Prevalence of the hypertriglyceridemic waist phenotype in Iranian adolescents. Am J Prev Med 2006; 30: 52-8.
PubMed ID: 16414424 CLOSE
CLOSE
Esmaillzadeh A, Mirmiran P and Azizi F. Whole-grain intake and the prevalence of hypertriglyceridemic waist phenotype in Tehranian adults. Am J Clin Nutr 2005; 81: 55-63.
PubMed ID: 15640460 CLOSE
CLOSE
Bos G, Dekker JM and Heine RJ. Non-HDL cholesterol contributes to the “hypertriglyceridemic waist” as a cardiovascular risk factor: the Hoorn Study. Diabetes Care 2004; 27: 283-284.
PubMed ID: 14694012 CLOSE
CLOSE
Ma CM, Liu XL, Lu N, et al. Hypertriglyceridemic waist phenotype and abnormal glucose metabolism: a system review and meta-analysis. Endocrine 2019; 64: 469-485.
PubMed ID: 31065910 CLOSE
CLOSE
Ren Y, Lu X, Wang C, et al. Prevalence of hypertriglyceridemic waist and association with risk of type 2 diabetes mellitus: a meta-analysis. Diabetes Metab Res Rev 2016; 32: 405-412.
PubMed ID: 26417844 CLOSE
CLOSE
Ford ES, Mokdad AH and Giles WH. Trends in waist circumference among U.S. adults. Obes Res 2003; 11: 1223-31.
PubMed ID: 14569048 CLOSE
CLOSE
Arsenault BJ, Lemieux I, Després JP, et al. The hypertriglyceridemic-waist phenotype and the risk of coronary artery disease: results from the EPIC-Norfolk prospective population study. CMAJ 2010; 182: 1427-1432.
PubMed ID: 20643837 CLOSE
CLOSE
Gerstein HC and Yusuf S. Dysglycaemia and risk of cardiovascular disease. Lancet 1996; 347: 949-50.
PubMed ID: 8598762 CLOSE
CLOSE
Coutinho M, Gerstein HC, Wang Y, et al. The relationship between glucose and incident cardiovascular events. A metaregression analysis of published data from 20 studies of 95,783 individuals followed for 12.4 years. Diabetes Care 1999; 22: 233-40.
PubMed ID: 10333939 CLOSE
CLOSE
St-Pierre J, Lemieux I, Perron P, et al. Relation of the “hypertriglyceridemic waist” phenotype to earlier manifestations of coronary artery disease in patients with glucose intolerance and type 2 diabetes mellitus. Am J Cardiol 2007; 99: 369-73.
PubMed ID: 17261400 CLOSE
CLOSE
Kinosian B, Glick H and Garland G. Cholesterol and coronary heart disease: predicting risks by levels and ratios. Ann Intern Med 1994; 121: 641-7.
PubMed ID: 7944071 CLOSE
CLOSE
Lemieux I, Lamarche B, Couillard C, et al. Total cholesterol/HDL cholesterol ratio vs LDL cholesterol/HDL cholesterol ratio as indices of ischemic heart disease risk in men. The Quebec Cardiovascular Study. Arch Intern Med 2001; 161: 2685-92.
PubMed ID: 11732933