In the past several decades, China has been experiencing rapid economic and social development with concomitant shifts in lifestyle habits and dietary structure. These changes have led to remarkable nutritional and epidemiologic transitions [1]. In particular, traditional dietary patterns are being lost as the population adapts to more industrialized and urban food environments [2]. At the same time, built living environments have become increasingly sedentary as a result of the unprecedented pace of urbanization. These changes have a significant impact on type 2 diabetes risk by increasing body weight and adiposity, and decreasing physical activity levels [3]. Meanwhile, these changes have resulted in a shift of public health priorities from infectious diseases to chronic diseases and from undernutrition to overnutrition and obesity. However, like many developing countries undergoing rapid nutrition transition, China is still facing coexisting problems of over- and undernutrition.
Obesity and diabetes trends
Obesity and diabetes were rare in the 1970’s in China prior to the economic reform. However, the past 3 decades have witnessed a sharp increase in prevalence of both obesity and type 2 diabetes, especially in urban areas. In a 2000-2001 nationally representative cross-sectional survey of 15,540 Chinese adults aged 35-74 years, the age-standardized prevalence of overweight or obesity was 26.9% in men and 31.1% in women [4]. In both urban and rural areas, the prevalence of underweight (BMI<18.5 kg/m2) decreased substantially, whereas the prevalence of overweight increased dramatically from 1989 to 2004 [5].
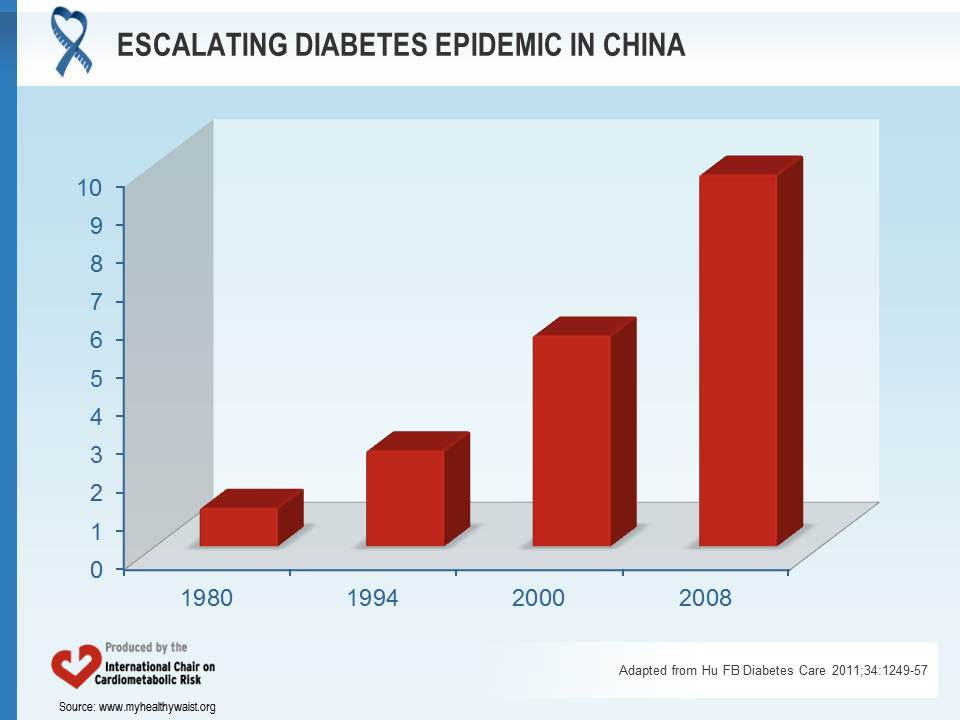
In parallel with the increasing obesity epidemic, the prevalence of type 2 diabetes is rising rapidly in China. Between 1980 and 2001, the prevalence of diabetes in Chinese adults increased from 1% to more than 5% [6]. The epidemics of obesity and diabetes are developing much faster in China than in the West. In 2008, the prevalence of diabetes reached nearly 10% in Chinese adults and it was estimated that more than 92 million Chinese had diabetes [7] (Figure 1). If no effective measures are taken to curb its growth, the number of people with diabetes will double in coming decades.
Perhaps the most alarming trend is a dramatic increase in childhood obesity. This coincides with a steep drop in the numbers of underweight children less than 5 years of age [8]. In 2005, the prevalence of childhood obesity in the northern metropolitan areas of China reached 32.5% for boys and 17.6% for girls aged 7-18 years old. This high prevalence of childhood obesity has important implications for the development of chronic diseases in adulthood.
Changes in dietary patterns
The nutrition transition typically involves increased consumption of animal fat and energy-dense foods, decreased fibre, and more frequent intake of fast foods. Between 1992 and 2002, the proportion of energy from animal foods increased from 9.3% to 13.7%, while that from fats rose from 7.8% to 29.8% [9]. Based on data from the China Health and Nutrition Surveys, meat intake rose 56% between 1989 and 2000, with the increase occurring in both urban and rural areas. Consumption of cereals decreased considerably, while intake of vegetable oils climbed dramatically. At the same time, the traditional diets in China, which are largely based on polished white rice and refined wheat, have high glycemic index and glycemic load, an important risk factor for developing type 2 diabetes [10], especially in overweight and sedentary individuals. Salt consumption is high in Chinese diets, especially in the Northern part of China, contributing to increased prevalence of hypertension and cardiovascular disease.
Fast food and soft drink consumption
One of the most profound results of globalization has been the rapid rise in the number of Western-style fast food outlets around the world [3]. The world’s largest fast food restaurant company, Yum! Brands Inc., operates nearly 38,000 restaurants (including KFC and Pizza Hut) around the world in more than 110 countries and territories, with over 4,650 fast food outlets in China [11]. Globally, there are more than 33,000 McDonald’s outlets in 119 countries and territories, serving around 68 million customers daily [12]. In China alone, the number of McDonald’s outlets grew from 1 in 1990 to 1,000 in 2006, and the company has plans to double this figure by 2013 [13].
In parallel with the growth of fast food consumption, sales of carbonated soft drinks have soared in China [14]. A rapid increase in the consumption of added sugar in the form of soft drinks is a major characteristic of nutrition transitions in developing countries [3].
Soft drinks high in glycemic load and empty calories play an important role in the development of obesity and diabetes. Data from epidemiological and experimental studies have shown that greater consumption of sugar-sweetened beverages (SSBs) is associated with weight gain and obesity in children and adults [15].
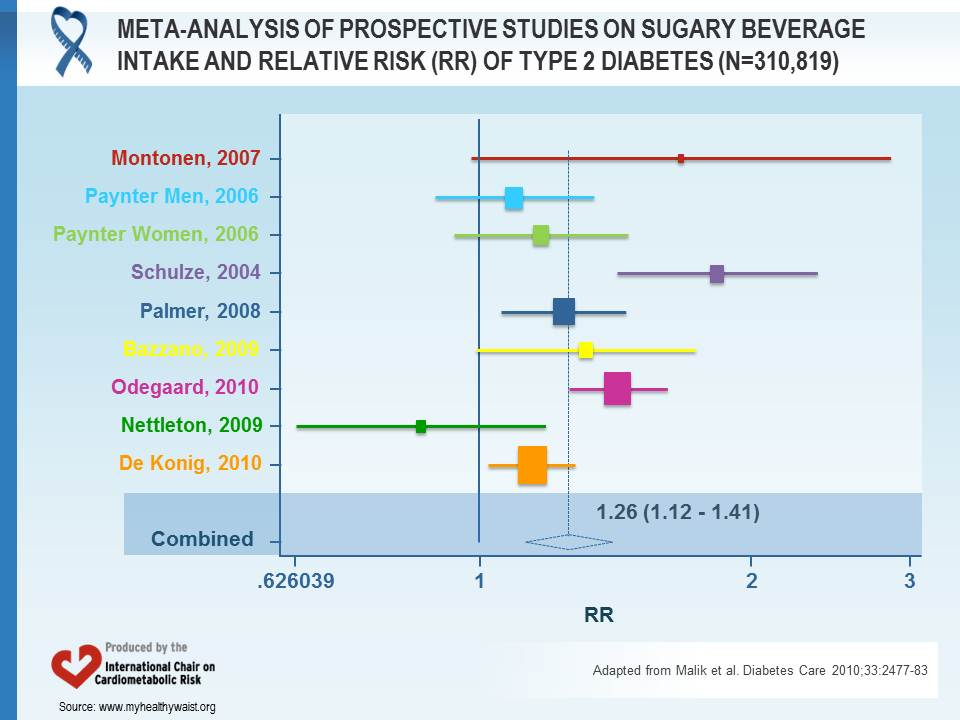
Evidence also indicates that higher consumption of SSBs increases the risk of type 2 diabetes even after taking into account the effects of body weight. A meta-analysis found that those in the highest quantile of SSB intake (most often 1-2 servings/day) had a 26% greater risk of developing the disease than those in the lowest (relative risk [RR]=1.26, 95% CI: 1.12-1.41) (Figure 2) [16]. In the Nurses’ Health Study II, those who consumed ≥1 SSB per day had an 83% greater risk of developing type 2 diabetes over the course of 8 years compared to those who drank <1/month (RR=1.85, 95% CI: 1.42-2.36; p<0.001 for trend) [17]. After adjusting for body mass index, the RR for extreme categories of intake decreased to 1.41 (95% CI: 1.09-1.83; p<0.001 for trend), but was still statistically significant. This suggests that the increased risk of diabetes was not completely explained by body mass index.
Several mechanisms in addition to weight gain may explain the adverse effects of SSBs on cardiometabolic risk. Large quantities of rapidly absorbable carbohydrates (e.g., sucrose) in SSBs result in a high dietary glycemic load that leads to quick increases in blood glucose and insulin levels. A high glycemic load diet, which increases insulin demand and may lead to pancreatic beta-cell exhaustion in the long run, has been implicated in increased risk of type 2 diabetes and cardiovascular disease [18]. Fructose from high fructose corn syrup or any sugar may also play a role. It is preferentially metabolized to lipid in the liver, leading to increased hepatic de novo lipogenesis, dyslipidemia, and insulin resistance. It may also promote intra-abdominal (visceral) adiposity. A study that compared the effects of consuming 25% of energy from glucose- or fructose-sweetened beverages showed similar weight gain, but only the fructose group had a significant increase in visceral adiposity [19].
Prevention strategies
Intervention studies have shown that diet and lifestyle interventions are effective in preventing type 2 diabetes [2]. In the Da Qing Diabetes Prevention Study conducted in China, after 6 years of active intervention, diabetes risk was reduced by 31%, 46%, and 42% in the diet only, exercise only, and diet plus exercise groups, respectively, compared to the control group [20]. In a subsequent 14-year follow-up study, the intervention groups were combined and compared to controls to assess how long the benefits of lifestyle change can extend beyond the period of active intervention [21]. Compared to controls, individuals in the combined lifestyle intervention group had a 51% lower risk of diabetes during the active intervention period, and a 43% lower risk over a 20-year follow-up. This study provides strong evidence to support long-term benefits of dietary and lifestyle interventions.
Over the past few decades, several population-based studies have been conducted in China to reduce risk of hypertension and other chronic conditions [1]. These have been implemented in communities, clinics, and worksites. These studies demonstrate that behaviour changes through health education and blood pressure control can reduce the burden of chronic diseases in China. However, few policy initiatives are in place to improve nutrition and physical activity.
Sound nutritional policies are critical for changing the unhealthy food environment [22]. To help consumers make informed dietary decisions, regulations should be put in place to require clear labelling of calorie, trans fat, sugar, and sodium content for all foods sold in containers or packages, including fast foods. However, food labels need to be preceded and/or accompanied by mass media campaigns to teach the general public how to use them, and why. Without education, nutrition labelling is unlikely to be an effective way to change food consumption patterns.
Food marketing can influence what foods an individual prefers, buys, and eats [23]. Children are particularly vulnerable to the influence of aggressive and misleading advertisement by food and beverage companies. Thus, governments and industries should reduce the amount of advertising and marketing of unhealthy foods to children. Legislation and regulations that restrict campaigns aimed at children through TV or other media are required to reduce the negative impact of junk food (e.g., sugary drinks and nutrient poor, energy-dense snacks) marketing [23].
Chronic disease risk factors can be successfully addressed through population-wide interventions and policy strategies to improve diet and increase physical activity [1]. Policy interventions, in particular, can bring about rapid and effective changes in nutrition and the physical environments. Both central and local governments should allocate more funding to create environments that enhance physical and psychological quality of life. In the past, China has successfully controlled acute infectious diseases through high-level policy interventions and a political system that allows for effective coordination and implementation. Similar strategies can be used to address the emerging epidemic of chronic diseases, which are exerting an increasingly heavy toll on public health and the economy.
References
- Hu FB, Liu Y and Willett WC. Preventing chronic diseases by promoting healthy diet and lifestyle: public policy implications for China. Obes Rev 2011; 12: 552-9. PubMed ID: 21366840
- Hu FB. Globalization of diabetes: the role of diet, lifestyle, and genes. Diabetes Care 2011; 34: 1249-57. PubMed ID: 21617109
- Pan A, Malik VS and Hu FB. Exporting diabetes mellitus to Asia: the impact of Western-style fast food. Circulation 2012; 126: 163-5. PubMed ID: 22753305
- Gu D, Reynolds K, Wu X, et al. Prevalence of the metabolic syndrome and overweight among adults in China. Lancet 2005; 365: 1398-405. PubMed ID: 15836888
- Zhai F, Wang H, Du S, et al. Lifespan nutrition and changing socio-economic conditions in China. Asia Pac J Clin Nutr 2007; 16 Suppl 1: 374-82. PubMed ID: 17392135
- Gu D, Reynolds K, Duan X, et al. Prevalence of diabetes and impaired fasting glucose in the Chinese adult population: International Collaborative Study of Cardiovascular Disease in Asia (InterASIA). Diabetologia 2003; 46: 1190-8. PubMed ID: 12879248
- Yang W, Lu J, Weng J, et al. Prevalence of diabetes among men and women in China. N Engl J Med 2010; 362: 1090-101. PubMed ID: 20335585
- Chen CM. Overview of obesity in Mainland China. Obes Rev 2008; 9 Suppl 1: 14-21. PubMed ID: 18307694
- Wang Y, Mi J, Shan XY, et al. Is China facing an obesity epidemic and the consequences? The trends in obesity and chronic disease in China. Int J Obes (Lond) 2007; 31: 177-88. PubMed ID: 16652128
- Sun Q, Spiegelman D, van Dam RM, et al. White rice, brown rice, and risk of type 2 diabetes in US men and women. Arch Intern Med 2010; 170: 961-9. PubMed ID: 20548009
- Yum! Brands Company. https://www.yum.com/wps/portal/yumbrands/Yumbrands/. Accessed March 2, 2020.
- McDonald’s. www.aboutmcdonalds.com/mcd/our_company.html. Accessed November 30, 2012.
- Fung E. McDonald’s to double restaurants in China. Wall Street Journal Online. March 29, 2010. online.wsj.com/article/SB10001424052702303601504575153702832556686.html. Accessed November 30, 2012.
- Kleiman S, Ng SW and Popkin B. Drinking to our health: can beverage companies cut calories while maintaining profits? Obes Rev 2012; 13: 258-74. PubMed ID: 22070346
- Malik VS, Schulze MB and Hu FB. Intake of sugar-sweetened beverages and weight gain: a systematic review. Am J Clin Nutr 2006; 84: 274-88. PubMed ID: 16895873
- Malik VS, Popkin BM, Bray GA, et al. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes Care 2010; 33: 2477-83. PubMed ID: 20693348
- Schulze MB, Manson JE, Ludwig DS, et al. Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. JAMA 2004; 292: 927-34. PubMed ID: 15328324
- Malik VS, Popkin BM, Bray GA, et al. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation 2010; 121: 1356-64. PubMed ID: 20308626
- Stanhope KL, Schwarz JM, Keim NL, et al. Consuming fructose-sweetened, not glucose-sweetened, beverages increases visceral adiposity and lipids and decreases insulin sensitivity in overweight/obese humans. J Clin Invest 2009; 119: 1322-34. PubMed ID: 19381015
- Pan XR, Li GW, Hu YH, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care 1997; 20: 537-44. PubMed ID: 9096977
- Li G, Zhang P, Wang J, et al. The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a 20-year follow-up study. Lancet 2008; 371: 1783-9. PubMed ID: 18502303
- Willett W, Koplan J, Nugent R, et al. Prevention of chronic disease by means of diet and lifestyle changes. Disease control priorities in developing countries 2006; 833-50. NCBI Book ID: BK11795
- Hawkes C. Regulating and litigating in the public interest: regulating food marketing to young people worldwide: trends and policy drivers. Am J Public Health 2007; 97: 1962-73. PubMed ID: 17901436