In recent decades, consumption of sugar-sweetened beverages (SSBs) has been rising rapidly worldwide. SSBs include the full spectrum of soft drinks (soda), fruit drinks, and energy and vitamin water drinks. In the US between the late 1970’s and 2001 the percentage of total calories consumed from SSBs increased from 3.9% to 9.2% [1]. Similar trends have been seen for Mexico, China, and India [1].
SSBs have become the primary source of added sugars in the US diet. They are also a major source of excess calories. Epidemiologic studies have shown consistent positive associations between SSB intake and weight gain and obesity in both children and adults [2, 3]. In recent years, there is emerging evidence linking higher consumption of SSBs and the risk of type 2 diabetes mellitus (T2DM).
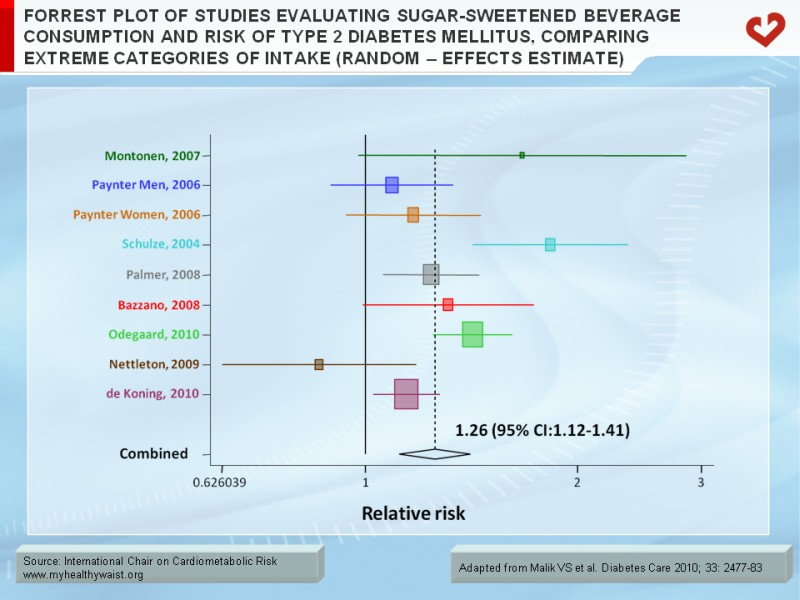
We have conducted a meta-analysis of prospective cohort studies of SSB consumption and risk of T2DM [4]. We identified 8 studies for inclusion in a random effects meta-analysis comparing SSB intake in the highest to lowest quantiles in relation to risk of T2DM. These studies included 310,819 participants and 15,043 cases of T2DM. In this meta-analysis, we found that individuals in the highest quantile of SSB intake (most often 1-2 servings/day) had a 26% greater risk of developing T2DM than those in the lowest quantile (none or <1 serving/month) [relative risk (RR)=1.26, 95% CI: 1.12-1.41] (Figure 1). Results from a dose-response meta-analysis indicated that increment in one 12-oz serving of SSB/day was associated with 25% increased risk of T2DM (95% CI: 1.10-1.42).
The two largest cohort studies published so far are the Nurses’ Health Study II (NHS II) and Black Women’s Health Study (BWHS). In the NHS II, a cohort of over 50,000 women, those who consumed ≥1 SSB per day had an 83% greater risk of developing T2DM over the course of 8 years compared to those who consumed <1 per month after adjusting for potential confounders (RR=1.85, 95% CI: 1.42-2.36, p<0.001 for trend) [5]. After further adjustment for body mass index (BMI), the RR comparing extreme categories of intake decreased to 1.41 (95% CI: 1.09-1.83, p<0.001 for trend), but was still statistically significant, suggesting that BMI accounts for about half of the excess risk. Similar results were reported in the BWHS. Among over 40,000 women followed for 10 years, those who consumed ≥2 SSBs per day had a 24% greater risk of developing T2DM compared to those who consumed <1 SSB per month (RR=1.24, 95% CI: 1.06-1.45, p=0.002 for trend) [6]. Additional adjustment for BMI resulted in a loss of statistical significance, suggesting that in this population, the majority of effect was mediated by BMI. In both cohort studies, increasing consumption of SSBs was associated with significantly greater weight gain, even after adjustment for other dietary and lifestyle factors.
Recently in the NHS, we found that a higher level of SSB intake was associated with increased risk of developing coronary heart disease (CHD) [7]. In over 88,000 women followed for 24 years, those who consumed ≥2 SSBs per day had a 35% greater risk of CHD compared to infrequent consumers, after adjusting for other unhealthy lifestyle factors (RR=1.35, 95% CI: 1.1-1.7, p<0.01 for trend). Additional adjustment for potential mediating factors including BMI, total energy intake and incident T2DM attenuated the associations but they remained statistically significant, suggesting that the effect of SSBs is not entirely mediated by these factors.
SSBs may lead to positive energy balance and weight gain due to decreased satiety and an incomplete compensatory reduction in energy intake at subsequent meals following intake of liquid calories. On average, one 12-oz serving of SSB contains about 140-150 calories. If these calories are added to the typical US diet without reducing calories from other sources, one SSB per day could lead to a weight gain of 15 lbs over the course of one year [3].
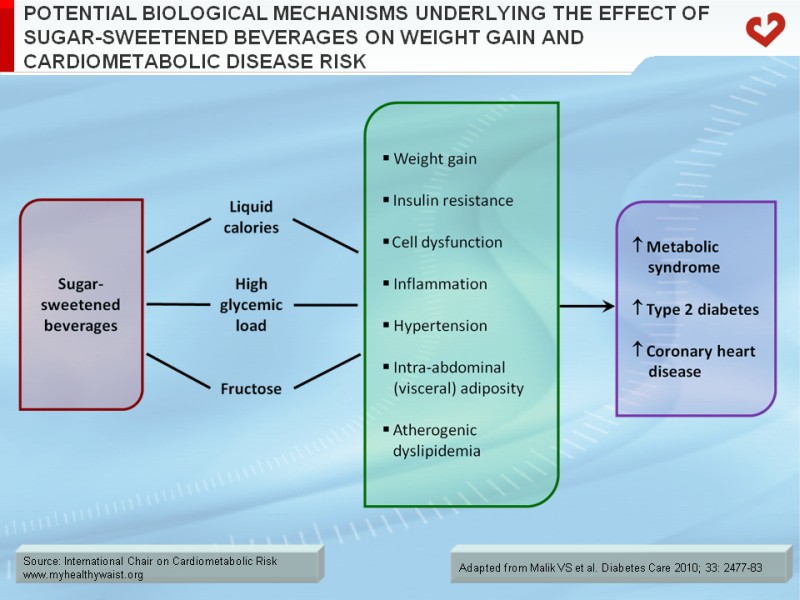
Metabolic consequences of SSB consumption may in part result from their propensity to induce weight gain, but the large quantities of rapidly absorbable carbohydrates such as sucrose or high-fructose corn syrup that are used to flavour these beverages, may also contribute to risk of T2DM (Figure 2). SSBs, which contribute to high dietary glycemic load (GL), induce rapid increases in blood glucose and insulin levels following consumption. Higher dietary GL has been associated with increased levels of inflammatory biomarkers such as C-reactive protein. A high GL diet has been also implicated in the increased risk of T2DM and CHD [1].
The fructose content of SSBs may exert additional adverse metabolic effects. Fructose is preferentially metabolized to lipid in the liver, leading to increased hepatic de novo lipogenesis, dyslipidemia and insulin resistance [8]. Fructose consumption has also been shown to promote accumulation of intra-abdominal (visceral) adiposity. In a recent study comparing the 10-week effects of consuming glucose- or fructose-sweetened beverages providing 25% of energy requirements, both groups showed similar weight gain, but only the fructose group showed a significant increase in intra-abdominal adiposity [9].
Given the strong epidemiologic and clinical evidence linking SSBs and increased risk of obesity and T2DM, limiting intake of SSBs is critical for primary prevention of these conditions in both children and adults. Recently, the American Heart Association recently released a scientific statement recommending reductions in added sugar intake to no more than 100-150 kcal per day for most American women and men respectively, as a means of reducing cardiovascular disease risk [10]. The statement identified SSBs as the primary source of added sugars in the American diet. Currently, a number of public health campaigns to limit intake of SSBs are underway and strategies such as taxation are currently being considered as a means of reducing intake of SSBs. Although many factors contribute to a growing pandemic of obesity and T2DM, ample evidence exists to discourage consumption of SSBs in place of healthy alternatives such as water, to reduce risk of obesity and T2DM.
References
- Malik VS, Popkin BM, Bray GA, et al. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation 2010; 121: 1356-64. PubMed ID: 20308626
- Hu FB and Malik VS. Sugar-sweetened beverages and risk of obesity and type 2 diabetes: epidemiologic evidence. Physiol Behav 2010; 100: 47-54. PubMed ID: 20138901
- Malik VS, Schulze MB and Hu FB. Intake of sugar-sweetened beverages and weight gain: a systematic review. Am J Clin Nutr 2006; 84: 274-88. PubMed ID: 16895873
- Malik VS, Popkin BM, Bray GA, et al. Sugar Sweetened Beverages and Risk of Metabolic Syndrome and Type 2 Diabetes: A Meta-analysis. Diabetes Care. 2010; 33: 2477-83. PubMed ID: 20693348
- Schulze MB, Manson JE, Ludwig DS, et al. Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. JAMA 2004; 292: 927-34. PubMed ID: 15328324
- Palmer JR, Boggs DA, Krishnan S, et al. Sugar-sweetened beverages and incidence of type 2 diabetes mellitus in African American women. Arch Intern Med 2008; 168: 1487-92. PubMed ID: 18663160
- Fung TT, Malik V, Rexrode KM, et al. Sweetened beverage consumption and risk of coronary heart disease in women. Am J Clin Nutr 2009; 89: 1037-42. PubMed ID: 19211821
- Stanhope KL and Havel PJ. Fructose consumption: recent results and their potential implications. Ann N Y Acad Sci 1190: 15-24. PubMed ID: 20388133
- Stanhope KL, Schwarz JM, Keim NL, et al. Consuming fructose-sweetened, not glucose-sweetened, beverages increases visceral adiposity and lipids and decreases insulin sensitivity in overweight/obese humans. J Clin Invest 2009; 119: 1322-34. PubMed ID: 19381015
- Johnson RK, Appel LJ, Brands M, et al. Dietary sugars intake and cardiovascular health: a scientific statement from the American Heart Association. Circulation 2009; 120: 1011-20. PubMed ID: 19704096