Hypertension
Defining CMR - Epidemiology - Traditional Modifiable CVD Risk FactorsKey Points
- The relationship between blood pressure and CVD events is continuous, consistent, and independent of other risk factors.
- The higher the blood pressure, the greater the chance of heart attack, heart failure, stroke, and kidney disease.
- Hypertension prevalence varies with sex and ethnicity and increases with age.
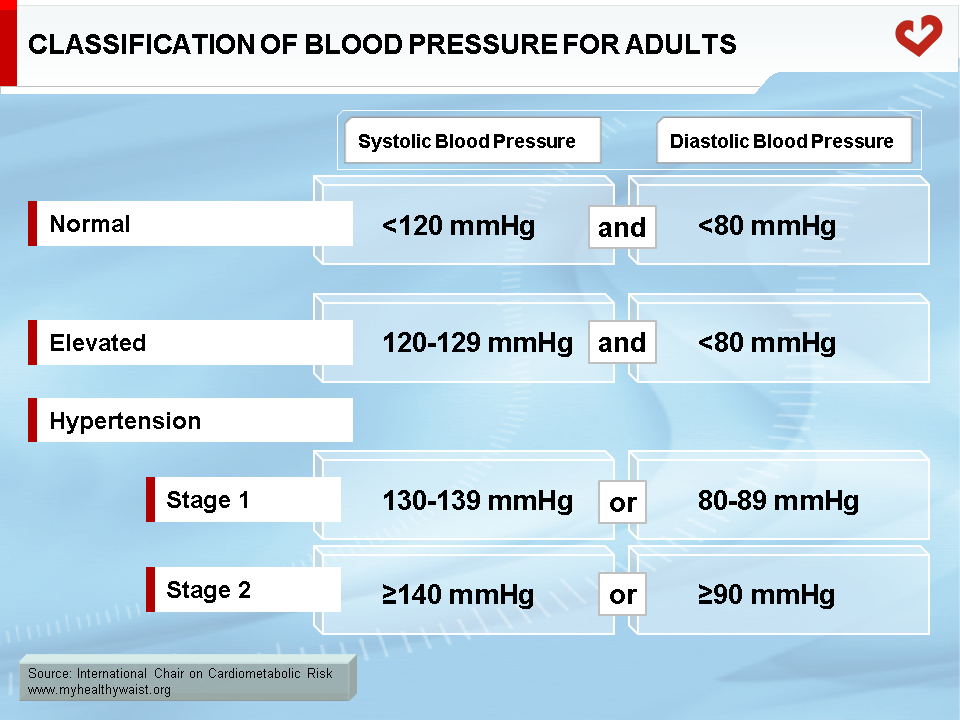
Blood Pressure Classification
Hypertension is one of the traditional modifiable cardiovascular disease (CVD) risk factors [1]. Stage 1 hypertenson is defined as systolic blood pressure (BP) between 130-139 mmHg or diastolic BP between 80-89 mmHg while stage 2 hypertension is defind as systolic BP ≥140 mmHg or diastolic BP ≥90 mmHg [1]. Normal and desirable BP values should fall below 120/80 mmHg (Table). The elevated stage is a critical step forward for healthcare professionals by enabling them to take action to prevent their patients from eventually progressing to full-blown hypertension [1].
Prevalence of Hypertension
Using data from the National Health and Nutrition Examination Survey (NHANES 2013-2016), the age-adjusted prevalence of hypertension among adults (≥20 years of age) in the United States was 46.0% (49.0% for men and 42.8% for women) [2]. Moreover, according to the National Vital Statistics System, there were 90,098 deaths primarily attributable to high BP in 2017 [2]. Hypertension prevalence varies with ethnicity, sex, and age. In the United States, the highest prevalence of hypertension was found in black men and women. Age-adjusted prevalence of hypertension among non-Hispanic black men was 57.6% and 53.2% among non-Hispanic women [2]. In both sexes, the prevalence of hypertension was reported to increase with age and was higher in men than in women up to 64 years of age [2]. Beyond this age, the prevalence of hypertension was found to be greater in women than in men [2]. Several other interesting statistics on high BP can be found in a report from the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines [1] and a report from the American Heart Association [2].
Complications of Hypertension
Hypertension is one of the most important modifiable risk factors for coronary heart disease, stroke, congestive heart failure, renal disease, and peripheral vascular disease. Arterial BP is a product of cardiac output and systemic vascular resistance. A number of factors modulate BP for adequate tissue perfusion, including humoral mediators, vascular reactivity, circulating blood volume, vascular calibre, blood viscosity, cardiac output, blood vessel elasticity, and neural stimulation [3]. Although genetics appears to play a role in essential hypertension, the exact mechanism has not been established. Uncontrolled and prolonged elevation of BP can cause adverse changes to cardiac structure and function in two ways: directly by increased afterload and indirectly by associated neurohormonal and vascular changes. Accordingly, hypertension can damage various organs of the cardiovascular and central nervous system and is a frequent cause of renal disease.
Cardiac involvement in hypertension manifests as left ventricular hypertrophy, left atrial enlargement, aortic root dilatation, atrial and ventricular arrhythmias, systolic and diastolic heart failure, and ischemic heart disease (IHD) [3]. Cerebrovascular manifestations include hemorrhagic and atheroembolic stroke or encephalopathy [3]. Nephrosclerosis and microalbuminuria are also some of the possible complications of long-standing hypertension in the kidney [3].
Hypertension and CVD
Data on more than one million individuals has shown that death from both IHD and stroke increases progressively and linearly from BP levels as low as 115/75 mmHg [4]. Beginning at 115/75 mmHg, every 20/10 mmHg increase in BP doubles the rate of mortality from both IHD and stroke [4]. In addition, longitudinal observations from the Framingham Heart Study have shown that BP values from 130/85 to 139/89 mmHg increase CVD risk more than twofold when compared to BP levels below 120/80 mmHg [5]. In addition, systolic BP has been reported to be a more important CVD risk factor than diastolic BP. Indeed, higher systolic BP was associated with increased CVD risk after statistical adjustment for diastolic BP while diastolic BP was not consistently associated with CVD risk once adjustment for systolic BP was performed [1].
In the Framingham study, Wilson et al. [6] followed a cohort of 3,323 middle-aged adults for the onset of CVD, CHD, and type 2 diabetes over an 8-year period. They reported that hypertension and HDL cholesterol contributed most to CVD outcomes. In addition, elevated BP was found to enhance the risk of myocardial infarction (MI) in populations with severe hypercholesterolemia [7,8].
Effect of anti-hypertensive therapy on CVD risk
Adopting a healthy lifestyle is crucial to prevent hypertension. However, anti-hypertensive therapy is recommended when BP is over 140/90 mmHg. Data from clinical trials has shown that anti-hypertensive therapy can have a beneficial effect, reducing stroke incidence by 35-40%, MI by 20-25%, and heart failure by over 50% [9]. In patients with hypertension from 140/90 to 159/99 mmHg and additional cardiovascular risk factors, a 12 mmHg reduction in systolic BP over 10 years will prevent 1 death for every 11 patients treated [10]. For more information on anti-hypertensive therapy, please visit the Managing CMR section.
Hypertension and Obesity
The worldwide obesity epidemic may have helped raise hypertension rates, as overweight individuals have higher rates of hypertension than normal weight individuals [11,12,13]. A weight loss of just 4.5 kg reduces BP and/or prevents hypertension in a large proportion of overweight individuals [14]. High BP is also a common feature of the metabolic syndrome, which increases the risk of developing CVD and type 2 diabetes. The link between hypertension and CVD may therefore be obesity, especially visceral obesity, which has been tied to various atherogenic and diabetogenic abnormalities [15]. For more information on visceral adipose tissue and hypertension, click here.
Hypertension is taking on greater importance as a medical and public health issue. The relationship between hypertension and CVD risk is well documented. An elevated BP increases the risk of MI, heart failure, stroke, as well as kidney and cerebrovascular diseases. Furthermore, hypertension is typically associated with abnormal cholesterol levels, a greater body mass index, and an increased prevalence of diabetes. Various hypertension management strategies are available to patients with elevated BP, including lifestyle modifications and antihypertensive drugs. However, healthcare professionals must not only identify and treat patients with hypertension, they must also promote a healthy lifestyle and emphasize prevention in order to decrease the prevalence of hypertension in the general population.
References
-
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation 2018; 138: e484-e594
PubMed ID: 30354654
-
Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke statistics-2020 update: a report from the American Heart Association. Circulation 2020;141:e139–e596.
PubMed ID: 31992061
-
Alexander AR, Madhur MS, Harrison DG, et al. Hypertension. Medscape, February 22, 2019. https://emedicine.medscape.com/article/241381
PubMed ID:
-
Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360: 1903-13
PubMed ID: 12493255
-
Vasan RS, Larson MG, Leip EP, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med 2001; 345: 1291-7
PubMed ID: 11794147
-
Wilson PW, D’Agostino RB, Parise H, et al. Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation 2005; 112: 3066-72
PubMed ID: 16275870
-
Kannel WB, Castelli WP and Gordon T. Cholesterol in the prediction of atherosclerotic disease. New perspectives based on the Framingham Study. Ann Intern Med 1979; 90: 85-91
PubMed ID: 217290
-
Salonen JT, Puska P and Kottke TE. Smoking, blood pressure and serum cholesterol as risk factors of acute myocardial infarction and death among men in Eastern Finland. Eur Heart J 1981; 2: 365-73
PubMed ID: 7333296
-
Neal B, MacMahon S and Chapman N. Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomised trials. Blood Pressure Lowering Treatment Trialists’ Collaboration. Lancet 2000; 356: 1955-64
PubMed ID: 11130523
-
Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42: 1206-52.
PubMed ID: 14656957
-
Brown CD, Higgins M, Donato KA, et al. Body mass index and the prevalence of hypertension and dyslipidemia. Obes Res 2000; 8: 605-19
PubMed ID: 11225709
-
Chiang BN, Perlman LV and Epstein FH. Overweight and hypertension. A review. Circulation 1969; 39: 403-21
PubMed ID: 4885946
-
Stamler R, Stamler J, Riedlinger WF, et al. Weight and blood pressure. Findings in hypertension screening of 1 million Americans. JAMA 1978; 240: 1607-10
PubMed ID: 691146
-
He J, Whelton PK, Appel LJ, et al. Long-term effects of weight loss and dietary sodium reduction on incidence of hypertension. Hypertension 2000; 35: 544-9
PubMed ID: 10679495
-
Després JP and Lemieux I. Abdominal obesity and metabolic syndrome. Nature 2006; 444: 881-7
PubMed ID: 17167477
 CLOSE
CLOSE
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation 2018; 138: e484-e594
PubMed ID: 30354654 CLOSE
CLOSE
Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke statistics-2020 update: a report from the American Heart Association. Circulation 2020;141:e139–e596.
PubMed ID: 31992061 CLOSE
CLOSE
Alexander AR, Madhur MS, Harrison DG, et al. Hypertension. Medscape, February 22, 2019. https://emedicine.medscape.com/article/241381
PubMed ID: CLOSE
CLOSE
Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360: 1903-13
PubMed ID: 12493255 CLOSE
CLOSE
Vasan RS, Larson MG, Leip EP, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med 2001; 345: 1291-7
PubMed ID: 11794147 CLOSE
CLOSE
Wilson PW, D’Agostino RB, Parise H, et al. Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation 2005; 112: 3066-72
PubMed ID: 16275870 CLOSE
CLOSE
Kannel WB, Castelli WP and Gordon T. Cholesterol in the prediction of atherosclerotic disease. New perspectives based on the Framingham Study. Ann Intern Med 1979; 90: 85-91
PubMed ID: 217290 CLOSE
CLOSE
Salonen JT, Puska P and Kottke TE. Smoking, blood pressure and serum cholesterol as risk factors of acute myocardial infarction and death among men in Eastern Finland. Eur Heart J 1981; 2: 365-73
PubMed ID: 7333296 CLOSE
CLOSE
Neal B, MacMahon S and Chapman N. Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomised trials. Blood Pressure Lowering Treatment Trialists’ Collaboration. Lancet 2000; 356: 1955-64
PubMed ID: 11130523 CLOSE
CLOSE
Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42: 1206-52.
PubMed ID: 14656957 CLOSE
CLOSE
Brown CD, Higgins M, Donato KA, et al. Body mass index and the prevalence of hypertension and dyslipidemia. Obes Res 2000; 8: 605-19
PubMed ID: 11225709 CLOSE
CLOSE
Chiang BN, Perlman LV and Epstein FH. Overweight and hypertension. A review. Circulation 1969; 39: 403-21
PubMed ID: 4885946 CLOSE
CLOSE
Stamler R, Stamler J, Riedlinger WF, et al. Weight and blood pressure. Findings in hypertension screening of 1 million Americans. JAMA 1978; 240: 1607-10
PubMed ID: 691146 CLOSE
CLOSE
He J, Whelton PK, Appel LJ, et al. Long-term effects of weight loss and dietary sodium reduction on incidence of hypertension. Hypertension 2000; 35: 544-9
PubMed ID: 10679495 CLOSE
CLOSE
Després JP and Lemieux I. Abdominal obesity and metabolic syndrome. Nature 2006; 444: 881-7
PubMed ID: 17167477